Scientists are successfully experimenting with a creative approach to treat cancer by genetically programming bacteria to invade tumours and destroy cells from within.
In a study published this week in the journal Nature, authors showed programmed bacteria given to mice with aggressive liver cancer were able to destroy themselves while releasing a drug into the tumour at the same time.
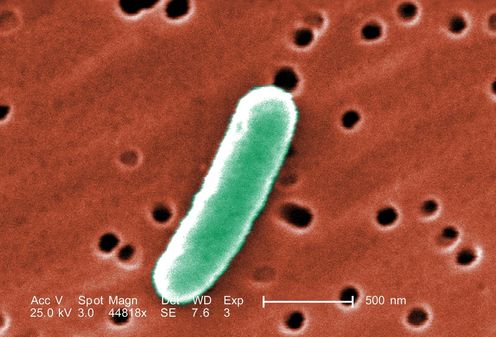
Researchers exploited the tumours’ poor blood supply, and consequently poor oxygen levels, by using strains of Salmonella enterica (S. enterica) – a bacterial species that can survive when no oxygen is present. The bacteria was drawn to the low-oxygen environment inside the tumour and provided targeted destruction of diseased cells.
Differentiating cancer cells from normal cells is critical to reduce the often awful side-effects of chemotherapy that come about because healthy cells are affected alongside cancerous ones.
The study’s authors showed when this treatment was provided alongside chemotherapy in mice, tumours shrank significantly within 18 days before regrowing.
The use of the engineered bacteria alongside chemotherapy was significantly more effective than chemotherapy alone, but substantial development of this technology is required before it can be employed in humans.
Bacteria and cancer
Traditional cancer treatments such as chemotherapy and surgery have made great strides towards better patient outcomes. Yet we are increasingly recognising the need for new ideas and technologies if we want to truly defeat cancer.
Bacteria are single-celled microorganisms that live everywhere that life exists on earth, including our own bodies. Their cells are around ten times smaller than our own, which means if a single engineered bacterial cell were to attack a tumour, it would have little or no effect.
Therefore, the study’s authors programmed bacteria to effectively count themselves and only attack the tumour when they had the numbers to be effective. This was done using a naturally occurring system called “quorum sensing” where individual cells emit a signalling molecule into the environment.
When there are few other cells in the near vicinity, the signalling molecules exist at a low concentration. As bacterial cells grow and divide, they make more and more of the signalling molecule until it reaches a critical concentration at which every cell in the population simultaneously switches on groups of genes.
In this case, the bacteria turn on genes that result in a self-destruct program. Nearly all the bacterial cells in the population rupture to release an anti-cancer drug called Haemolysin E into the tumour. The drug kills cancer cells by puncturing their membranes and therefore making holes for their inner components to leak out of.
The few bacterial cells that don’t execute the self-destruct function grow again to repeat the process so cycles of tumour attacks are repeated.
Synthetic biology
Bacteria were suggested for use in cancer treatment as early as 1891, but without the tools of synthetic biology this approach would be impossible. Synthetic biologists combine principles from engineering, molecular biology and computer science to reprogram living organisms to perform useful functions.
For example, synthetic biology is being used to engineer microorganisms to produce bio-fuels and chemicals from renewable resources, produce pharmaceuticals and novel drugs and even execute computational tasks for a variety of applications.
Bacteria have evolved to be efficient at replication, and performing functions desired by humans, such as coordinated tumour destruction, is not normally part of their behavioural repertoire. But synthetic biology provides the means to encode entirely new functions in microorganisms with the fine level of control demanded by modern engineering disciplines.
Of course several steps need to be taken before the treatment method shown in the Nature study can become a reality. The efficiency of the engineered bacterial cells’ tumour-destroying abilities would need to be dramatically improved to prevent regrowth.
Another consideration is that at the moment there is no mechanism that would prevent the bacteria from evolving to live outside the low-oxygen tumour environment and attacking other parts of the body.
Although this scenario is unlikely because the bacteria would have to compete with the trillions of naturally occurring microorganisms that thrive in the human body, issues like this would need to be addressed before proceeding to further trials.
On the bright side, synthetic biologists are more than capable of engineering the safety mechanisms that would be required to advance this technology to the clinic.
Thomas Williams does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond the academic appointment above.