A MELBOURNE discovery has given the first hope in 30 years of beating a cancer that kills half the infants it strikes.
A team led by the Peter MacCallum Cancer Centre has revealed two drugs being trialled in patients may be able to overcome acute myeloid leukaemia when combined.
About 100 of the 1000 Australians diagnosed with AML each year will be a baby, making it the most common cause of disease death for infants.
Almost half of all infants diagnosed with the AML sub type of the disease die, while only one in five adults diagnosed are alive after five years.
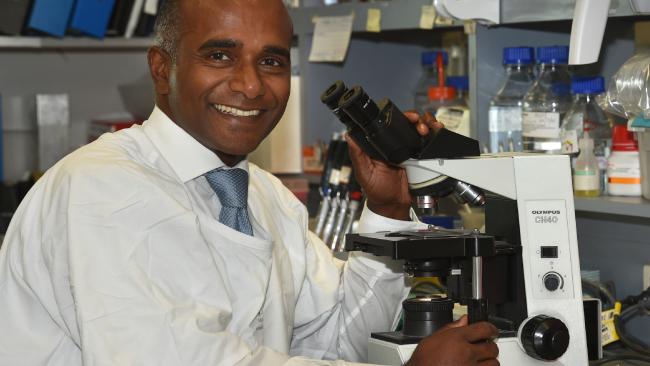
Working with international collaborators, Peter Mac’s Professor Mark Dawson discovered for the first time the role two proteins play in the regulation of the cancer.
While it was known that proteins BRD4 and DOT1L played an unknown but key role in regulating the leukaemia, Professor Dawson’s team established that the two depended on each other to progress the disease.
“We’ve never really known why this leukaemia, more than other subtypes of leukaemia, seem to respond so well to drugs that target these two proteins,” he said.
“This research tells us exactly how these two proteins work in this type of leukaemia, and then it actually gives us insight into the fact they talk to each other, and by doing so they collaborate with each other to drive the leukaemia.
“Potentially targeting both is a unique opportunity for us to go forward.”
Disrupting the two proteins so they cannot communicate could create a way of overcoming the disease, which has not seen a new treatment developed since the 1970s.
In a further boost, the breakthrough raises the importance of separate clinical trials already underway for two drugs which target each of the proteins and have shown individual promise in impacting but not overcoming leukaemia.
One drug showing promise in inhibiting the BRD4 protein is in clinical trials at Peter Mac, while another aimed at DOT1L is being trialled in patients in the US.
Professor Dawson’s research, published in the journal Nature Structural & Molecular Biology, has opened the door for new clinical trials bringing the two drugs together as a combined therapy, vastly multiplying their impact on the disease.
“It is not going to change things in the next year …(but) we don’t have to develop new drugs, we have drugs for these two proteins, and we now know they are safe and tolerable,” he said.
“We also know the drugs by themselves have some activity, but we have never been able to combine them before, so now we need to do that.”