
A growing glut of doctors has forced GPs to “chase patients” and pushed bulk-billing rates to record highs, leaving Medicare vulnerable to overuse that will add to its projected cost blowout of more than $35 billion within a decade.
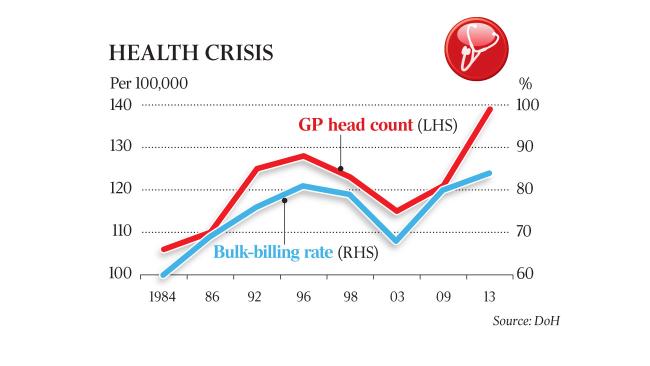
Growth in GP numbers of almost 50 per cent over the past decade — 2.5 times population growth — has undermined doctors’ ability to charge fees above the Medicare Benefits Schedule, according to Australian Population Research Institute analysis.
The findings cast doubt on Labor’s and doctors’ claims that the Coalition’s plan to freeze the MBS for a further two years until 2020, to save $925 million, would hit bulk-billing rates. “There are so many GPs seeking patients that few could risk charging a co-payment because patients would go around the corner to a competitor who bulk bills,” said report author Bob Birrell. “Oversupply is the cause of escalation of GP costs that the Coalition is trying to curtail. But freezing the rebate is just a Band-Aid.”
Growth in GP numbers of almost 50 per cent over the past decade — 2.5 times population growth — has undermined doctors’ ability to charge fees above the Medicare Benefits Schedule.
Mr Birrell called for a lowering of the intake of overseas-trained doctors and new limits on where doctors funded by Medicare were able to practise. While the population has increased 19 per cent since 2005, the number of GPs has surged 47 per cent to 33,275, including growth of more than 110 per cent among overseas-trained doctors, who tend to move to cities after completing mandatory stints in regional areas.
“There are no rules stopping overseas-trained doctors who have completed regional work requirements from moving, no matter how oversupplied their chosen location is,” Mr Birrell said. The number of overseas doctors practising in metropolitan areas jumped 112 per cent to 4520 over the decade to 2015, he said.
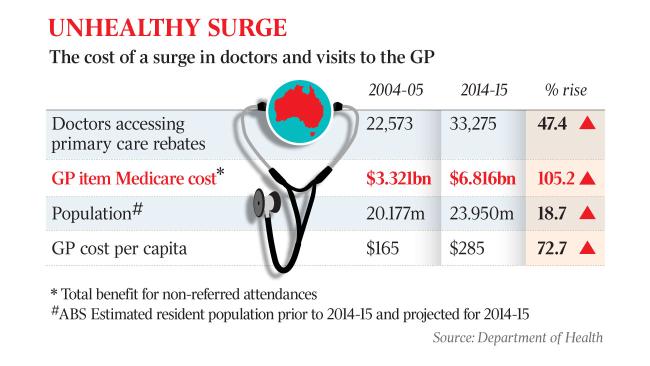
Bulk billing — where doctors agree to accept payment directly from Medicare rather than charge upfront fees — has increased from 75 per cent of GP visits in 2005 to a record high of about 85 per cent this year. Meanwhile, the annual cost to Medicare of non-referred doctor visits has more than doubled to $6.8bn — equivalent to a 73 per cent increase in the annual cost of GP services per person.
Labor has promised to unfreeze the MBS from next year, if it wins government, at a cost of $12bn over a decade, which has pleased doctors’ groups, who argue bulk-billing rates will fall if the rebate freeze — in place since 2013 — is allowed to continue under the Coalition.
Australian Medical Association president Michael Gannon said a growing GP workforce was a plus for Australia even if doctors were becoming excessively concentrated in some areas.
“GPs are the gatekeepers of the system and provide enormous value of money, being only about 6 per cent of national health costs,” Dr Gannon said. “There’s no question we’re much closer to having a maldistribution rather than oversupply.”
The study, which uses Department of Health data, argues a growing number of corporate practices are responsible for over-billing. “Corporates have been offering highly lucrative contracts on the condition that those employed accept their style of medicine — high throughput and bulk billing,” it said. Michael Wooldridge, a former long-serving health minister, said price gaps were a function of market power rather than the Medicare rebate, “and nothing else”. “About 1994, an increase in anaesthetic rebates led to greater gaps; ditto about 2000, when I was stupid enough to increase obstetric rebates,” Dr Wooldridge said. The latest internationally comparable OECD data shows the number of doctors per 1000 people in Australia has grown by 29 per cent to 3.4 over the decade to 2013 — more than twice as fast as the OECD average. Australia had significantly more doctors per 1000 people than the US, Canada, Britain and New Zealand, which each had fewer than 2.8. “Despite mounting evidence to the contrary, belief in a doctor shortage has developed a life of its own,” Mr Birrell said.
His co-author, Mike Moynihan, former president of the Rural Doctors Association of Victoria, said the doctor glut was fuelling frivolous visits. “People are coming in for a sniffle or to get documents signed. On the other hand, doctors are generating repeat visits by requesting tests that aren’t necessary,” he said.
The number of GP visits per person has increased more than 20 per cent over the decade to 5.7, the study shows. The cost of GP visits to Medicare (about one-third of the total cost) is projected to rise by 5 per cent a year over the next 10 years to $12.1bn, according to a Parliamentary Budget Office report. The 2014 commission of audit said health spending was the “commonwealth’s single largest long-run fiscal challenge”.