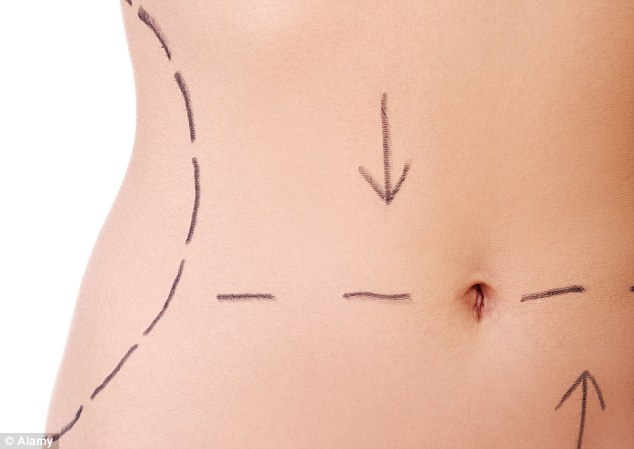
On Monday the Medical Board of Australia issued regulations for medical practitioners following wide consultation with the industry and the public about how to protect people undergoing cosmetic procedures.
The new regulations, which will take effect from October, prescribe a seven-day cooling off period for adults before major procedures. For anyone under 18 there will be a three-month cooling-off period before major procedures, with a mandatory evaluation by a registered psychologist, general practitioner or psychiatrist, and a seven-day cooling off period before minor procedures.
Treating medical practitioners will have to take “explicit responsibility for postoperative care and for making sure there are emergency facilities when they are using sedation, anaesthesia or analgesia”.
The vice president of the Australian Society of Plastic Surgeons, Dr Gazi Hussain, welcomed those requirements. But he said it did not change the fact that any doctor with a basic medical qualification could perform some potentially dangerous and invasive cosmetic operations.
“In our submission to the Medical Board we specifically requested there be a requirement for basic training in cosmetic surgery, and we would always recommend someone has training from the Royal Australasian College of Surgeons given the lack of regulation,” he said.
Medical doctors might be capable of making incisions and performing some surgeries, he said, but they might lack the training to respond if something went wrong. When procedures were carried out in non-licensed medical facilities, there were no specialists, such as anaesthetists or emergency doctors, on hand to respond. It is not illegal to conduct surgical procedures in an unaccredited facility, such as an office space, Hussain said.
“I’ve seen patients who have had branches of their facial nerves cut and I have had to try to repair or improve that; I’ve seen patients with breast implants who then come to emergency departments with infections, and I’ve had patients with tummy tucks falling apart,” Hussain said.
“Mostly it had been done by non-plastic surgeons.”
There have been calls for tougher regulations for plastic surgeons as well, and the new regulations will also apply to them. When complications from both cosmetic and plastic surgery occur, it can be difficult for patients to know if they are suffering a statistically unfortunate but genuine complication, or are a victim of malpractice.
Research by Marie Bismark, a doctor and lawyer, found that of nearly 10,000 Australian medico-legal cases resolved over a six-year period, 16% involved cosmetic procedures. Plastic surgeons, orthopaedic surgeons, vascular surgeons and dermatologists experienced disproportionately high rates of consent disputes, with patients feeling they were not given enough information to give informed consent, her study found.
As well as the cooling-off period, the new regulations contain explicit guidance on patient assessment and informed consent, and require doctors to provide clear information to consumers about costs, risks and possible complications.
“There were some concerns that benefits of some procedures were being oversold and that patients didn’t fully understand the risks or that it might not go as they believed.”
The chairwoman of the Medical Board of Australia, Dr Joanna Flynn, said cosmetic surgery was very broad and difficult to define, which hampered regulation. It included everything from non-surgical laser hair removal and Botox through to breast augmentation and other invasive procedures.
“These guidelines haven’t gone into the issue of specific qualifications, but not all the harm is done by those with less training,” she said.
“There was consideration about whether cosmetic surgery should be recognised as a speciality in its own right which would require certain specialisation, and that needs to happen before the Medical Board can implement a need for specific qualifications. But it didn’t meet the test requirements for making it a speciality, and that’s largely because it’s such a diverse field encompassing relatively minor to major procedures.”