Inhibiting the transfer of calcium ions into the cell’s powerhouse is specifically toxic to cancer cells, according to an article published this week in Cell Reports by researchers from the Perelman School of Medicine at the University of Pennsylvania.
“This suggests that calcium addiction by mitochondria is a novel feature of cancer cells,” said senior author Kevin Foskett, PhD, chair of the department of Physiology. “We were surprised by this unexpected dependency on calcium transfer to the mitochondria for the survival of cancer cells.” These findings suggest an entirely new target for cancer drugs.
Special proteins, called IP3Rs for short, are a common family of calcium ion channels that span the membranes of the endoplasmic reticulum (ER), a network of small tubes inside every cell that involved in making proteins and lipids. Calcium ions from the ER are released through the channel and regulate many cell functions, including cell metabolism. This is achieved primarily by supplying calcium to mitochondria where it stimulates the production of ATP to power cell functions.
Most healthy cells in the body rely on a complicated process called oxidative phosphorylation to produce ATP. Knowledge about how ATP is produced by the cell’s mitochondria, the energy storehouse, is important for understanding normal cell metabolism, which will provides insights into abnormal cell metabolism, as in the case of cancer.
The Foskett lab showed in a 2010 Cell article that a fundamental control system regulating ATP is an ongoing shuttling of calcium ions to the mitochondria from the ER, and this maintains normal levels of ATP in a wide variety of cell types. They also found that in the absence of this calcium ion transfer, ATP levels fall and a process called autophagy, literally self-eating, is induced so the cell can survive.
In all cell types that the team examined, inhibiting the uptake of calcium ions by mitochondria induced a bioenergetic crisis that reprogrammed the cells’ metabolism in a way that is reminiscent of nutrient starvation, despite nutrient availability and uptake by the cell. A hallmark of cancer cells is re-programming their own metabolism, even when nutrients are available to provide the building blocks necessary for cancer cells to divide and grow so prolifically. As such, all major tumor suppressors and oncogenes have connections with metabolic pathways.
“Accordingly, we asked what role calcium uptake by mitochondria plays in cancer cell metabolism and viability,” Foskett said. Using breast and prostate cancer cell lines and human fibroblast cells that were transformed into cancer cells, the team found that interrupting the transfer of calcium from the ER to the mitochondria diminished ATP production and induced autophagy, similar to that seen in normal cells. However, they also saw that while autophagy was sufficient for the survival of normal cells, it was insufficient for cancer cells. These cells responded with massive death while their normal counterparts survived. Providing metabolic substrates that are normally used in mitochondria to the cells rescued the lethal effect of inhibiting mitochondrial calcium uptake. “This suggests that cell death was induced by compromised bioenergetics,” Foskett explained.
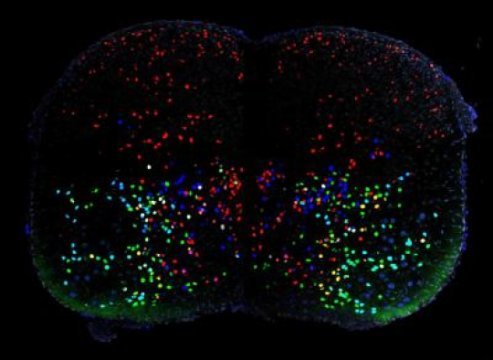
Inhibiting the activity of IP3R channels strongly suppressed melanoma tumor growth in mice. The team demonstrated that suppression of tumor growth was due to cell death caused by necrosis, which occurred at the time each cancer cell divided. Normal cells didn’t die when mitochondria could not take up calcium because they slowed their growth when their metabolism was compromised, avoiding death associated with cell division, whereas the cancer cells continued to try to grow and divide and suffered cell death as a consequence.
“Our findings reveal a fundamental and unexpected dependency by cancer cells on calcium transfer by IP3R channels into mitochondria for their viability,” Foskett said. “Mitochondria inside cancer cells are addicted to calcium. This addiction can now be considered as a target for new cancer therapies. Our studies suggest the existence of completely unexpected new targets for which drugs could be developed to kill cancer cells specifically by targeting calcium release from the ER and calcium uptake by mitochondria. A major challenge now is to discover drugs that can do this.”
Story Source:
The above post is reprinted from materials provided by University of Pennsylvania School of Medicine. Note: Materials may be edited for content and length.
Journal Reference:
- César Cárdenas et al. Selective Vulnerability of Cancer Cells by Inhibition of Ca2 Transfer from Endoplasmic Reticulum to Mitochondria. Cell Reports, March 2016 DOI:10.1016/j.celrep.2016.02.030