Nearly 200 people in the San Francisco area have been sickened by an intestinal disease caused by the highly contagious Shigella bacteria since an outbreak began at a Mexican seafood restaurant 10 days ago, health officials said today.
The outbreak, which began on Oct. 16 at the Mariscos San Juan No. 3 restaurant in San Jose, had spread across six counties and infected 190 people as of Wednesday night, the Santa Clara County Public Health Department said in a statement. Many of those sickened have required hospitalization and at least a dozen were admitted to intensive care units, health officials said.
As NBC South Bay reported:
“My fever was at 104 — that’s when vomiting started,” said Andres Guera, who was still recovering late Monday after spending the weekend in the intensive care unit at Kaiser Permanente hospital in Santa Clara. Guera said the pain started Friday after having lunch at Mariscos.
“The first thing they did was put seven liters of fluid in me,” Guera said. Guera soon found out he was not the only one sickened after an emergency room nurse told him “it was like a Hollywood movie down there with all the patients coming in.”
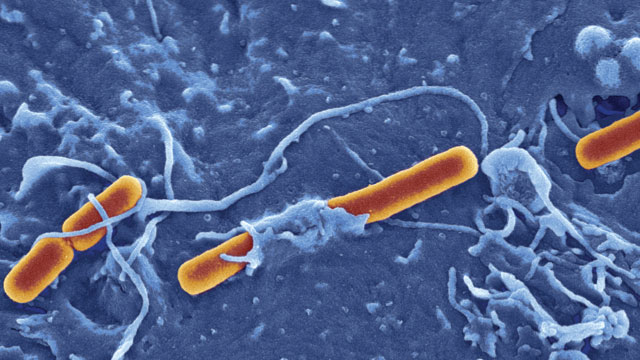
Transmission of Shigella bacteria typically occurs when fecal matter enters the mouth, possibly when an infected food handler prepares meals consumed by unwitting diners. Because the bacteria is resistant to gastric acid, a person can get infected with as little as 10 organisms. Sexual transmission may also occur, though it’s far less common. The health department said it is investigating all possible sources of the contamination.
According to the Centers for Disease Control and Prevention, infection with Shigella can trigger watery or bloody diarrhea, abdominal pain, fever and other symptoms. More serious complications — including seizures and toxemia –are possible, depending on the strain of Shigella. The bacteria is “extremely contagious,” health officials said, urging sickened individuals to avoid going to work.
Two lawsuits have been filed over the outbreak as of last Friday, according to the Marler Clark law firm. The restaurant, which has been closed since Oct. 18, is cooperating with the department’s investigation, health officials said.
Shigella bacteria cause some 500,000 cases of diarrheal disease in the United States every year, according to CDC figures. Symptoms usually last anywhere between five and seven days for people who have strong immune systems, although it can take months for an infected person’s gastrointestinal system to return to normal. People with weaker immune systems face greater risks if they are infected with Shigella. For young children, the elderly, and people infected with HIV, for instance, it can be life-threatening, although deaths caused by the bacteria are rare.
While Shigella infections were once easy to treat with antibiotics, drug-resistant strains are now becoming increasingly common in the United States, with more and more doctors finding that the drugs that once wiped out the infection are no longer effective. In 2014, for instance, nearly 90 percent of patients infected with Shigella had strains that were resistant to the antibiotic ciprofloxacin (Cipro), which usually is the first drug tried against shigellosis. Before last year, Cipro resistance was found in just 2 percent of Shigella infections tested in the US.
“Drug-resistant infections are harder to treat and because Shigella spreads so easily between people, the potential for more – and larger – outbreaks is a real concern,” CDC director Dr. Tom Frieden, M.D., M.P.H., said in April.
Drug resistance, which occurs when bacteria acquire genetic changes that give them the ability to withstand antibiotics, accounts for about 700,000 deaths around the world each year. The World Health Organization said last year that bacteria resistant to antibiotics have spread to every part of the world, and if left unchecked, will take us back to a “pre-antibiotic era” in which minor infections like strep throat could kill. By 2050, scientists predict that drug-resistant bacteria could kill as many as 10 million people annually.