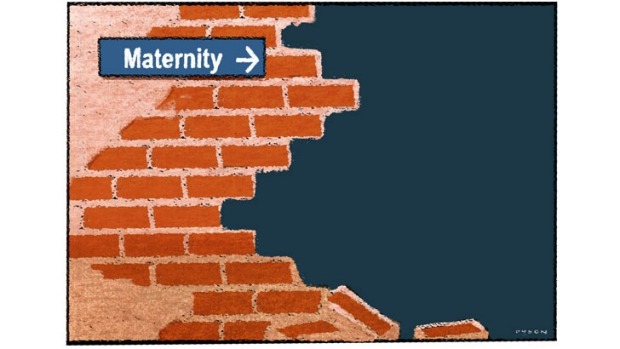
The revelations about avoidable infant deaths at Bacchus Marsh Hospital are only the tip of the iceberg of complications caused by substandard care.
For too long hospitals have been able to hide their poor outcomes behind excuses of confidentiality or policy.
If there were seven preventable deaths, it is almost certain that there have been multiple non-lethal complications affecting both mothers and babies. So this has proved, with many other mothers coming forward with their stories. Indeed I was already acting for one mother when the revelations came to light.
The failures that occurred at Bacchus Marsh Hospital, which is managed by Djerriwarrh Health Services, are endemic in the health system, but at Bacchus Marsh Hospital a perfect storm of individual factors combined to allow poor attitudes, inappropriate policies and negligent treatment to occur. The community has a right to ask, and must ask, how such injuries could occur in 2013 and 2014. The factors that caused these deaths must be dealt with.
So, what were the factors that contributed to these appalling outcomes?
One, there was a cavalier attitude to risk. Bacchus Marsh Hospital offers maternity care for “low-risk pregnancies”. As these tragic circumstances show, having an uncomplicated pregnancy is no guarantee of a safe delivery.

Birth is a fluid and evolving process. Complications can occur very rapidly and can require an urgent response, yet obvious signs of complications appear to have been ignored. The test of the quality of a health service is not whether it can cope with most circumstances, but how it manages emergencies.
It has been reported that the head of obstetrics, Dr Surinder Parhar?, did not favour interventions in birth. The delivery room is not a place for an individual’s medical ideology; it is a place for careful monitoring, listening to patients, and assessment of each individual mother and baby’s risks and needs.
Two, the health service was in a rural area. Access to quality maternity care should not depend on where you live. But the reality is it does. It can be difficult to recruit experienced, expert staff to rural areas, and the difficulty of replacing staff can foster a culture in which poor professional standards are tolerated. Rural women have a right to the same quality of care as their urban sisters.
Three, senior staff developed a God complex. Recent publicity about sexual harassment and bullying of junior surgeons by their superiors shows the unassailability of senior practitioners in the health system and the dysfunction this causes in the provision of quality care.
Midwives are trained to assess maternal and infant risks and they have much more contact with labouring women than obstetricians, so their opinions and recommendations should be treated with respect. Good medical care is provided where there are partnerships between doctors and other staff, not what is in effect a professional apartheid.
Four, the hospital ignored complaints and concerns by other workers, or rather, it discouraged reports at all, or punished staff for making them.
Media reports suggest that a culture of fear and intimidation flourished within Djerriwarrh Health Services. Bacchus Marsh Hospital discouraged reporting of adverse outcomes. This sends the wrong messages to staff and causes resignations, which then further compromises the available skills base. Most importantly opportunities to learn from mistakes were missed and then the mistakes repeated.
Five, the hospital abrogated its governance requirements. It is the responsibility of management to monitor performance and address any issues. Failure to do so is a fundamental failure in governance.
Six, it failed to consider demographic trends and plan for future needs. Djerriwarrh Health services cover one of the fastest growing areas in the state. Births at Bacchus Marsh Hospital have reportedly doubled in recent years. Inadequate resourcing and outdated equipment were undoubtedly a factor in the deaths and injuries at Djerriwarrh Health. Reports that some staff had poor foetal monitoring skills are alarming. Monitoring of the baby during labour and delivery is the mainstay of foetal safety.
Seven, the regulatory body responsible for complaints was hopelessly incompetent. The fact that it took 28 months to investigate a complaint against the head of obstetrics is completely unacceptable. The complaint was serious and indicated ongoing risks to patients. Babies died while the Australian Health Profession Regulation Agency (AHPRA) sat on its hands.
The starting point to reduce these risks is a culture of transparency. For too long hospitals have been able to hide their poor outcomes behind excuses of confidentiality or policy. Each death or adverse outcome is investigated by an internal review committee, but there is no requirement to report findings. The independence of internal reviews must also be questioned.
There also needs to be consistent and independent oversight. Internal reviews should be independently audited and made public. This will allow early detection of problems and swift remedial action. Patients and potential patients have the right to know about complication rates at their health service provider and to make informed decisions about their care.
A significant attitudinal change must also occur and the hierarchical structure of the health system must be challenged. Nurses, midwives and allied health workers have much to contribute to reform and patient safety, as well as patient care.
Finally, we need to challenge the reluctance of health professionals to report on each other. Dr Parhar was reported to AHPRA by a fellow doctor. In my experience, this is extremely unusual. There is an “everyone knows about Dr X” attitude, but no sense of responsibility to do anything about it. Unfortunately, the patients do not know about a doctor’s failings and are therefore unnecessarily exposed to risk. The ability of AHPRA to address serious complaints in a meaningful and timely manner must be urgently addressed.
The babies and women who have suffered deserve answers, and most importantly, their injuries must not be repeated.
Paula Shelton is a social justice and medical negligence lawyer with Shine Lawyers.