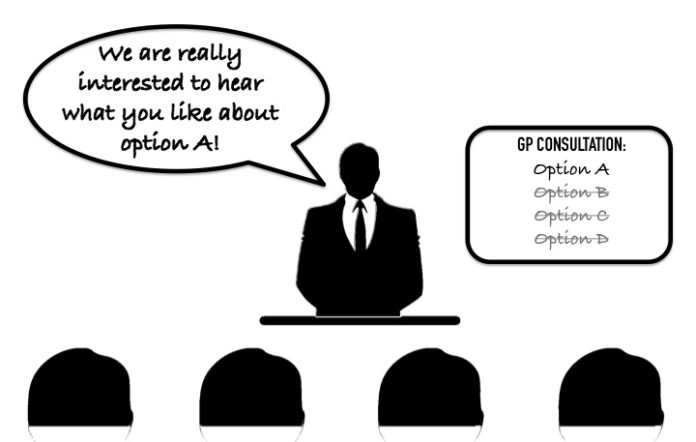
I had an interesting experience recently. I participated in a webinar organised by the Department of Health. It was supposed to be a consultation of GPs about the uptake of eHealth.
It went something like this: “We want to gain feedback from GPs about how we can get you to use the eHealth. This is how we’re going to do it; we’ve already organised training and we’re kicking off after the Christmas break. But before we start this session you must know that we cannot consider other options or timeframes.”
I was speechless. Literally – as I was not allowed to speak. I could only send little text messages via the closed online question platform. I was unable to see the feedback from other online participants.
Meaningful use?
For years health providers have repeated the same message over and over: if you want to make eHealth successful please take us with you.
The government is talking about new incentive payments to practices, ‘refreshed’ training programs and opt-out instead of opt-in, but there is little mention about improvements that make health providers want to use the PCEHR (now called ‘My Health Record’).
I find it concerning is that the current plan only encourages uploading of documents. What should be facilitated is safe and more efficient care for our patients. At the moment it seems to be all about the number of uploads to the system. I cannot help but wonder what higher level performance indicators are at work here.
Any incentive has to be effective at provider level to create a behavioural change. In other words, we must encourage individual practitioners to use eHealth, not just organisations and practices.
It is no surprise that the government failed again to enlist support from the profession. In its submission to the Department of Health, the RACGP wrote:
“(…) the RACGP cannot support the proposed mandatory requirements for the uploading of a specified quota of clinical documents to My Health Record. Meaningful use is not just uploading information to My Health Record, and nor is uploading information an acceptable starting point for meaningful use. Meaningful use relates to safety, quality, communication and healthcare outcomes – not merely numbers.
Unresolved issues
E-health experts have warned that the system is still unsafe. For example, some software programs merge medication dose and instructions. Others have warned that the uploaded clinical information does not always arrive in the My Health Record database.
Then there are the unanswered medicolegal issues. For example, we still need clarification about some of the basics, including the purpose of the system. This is essential if we want to encourage meaningful use of eHealth.
As I wrote in MJA Insight, I would be happy if the data in My Health Record was used for other purposes such as disease surveillance or even feedback on my clinical management but, in the end, it is the patient’s record and they must have a say in it. A proper consent procedure is essential for any use of PCEHR data outside individual patient care.
It appears the system operator is currently authorised to collect information in individual health records for law enforcement, health provider indemnity insurance cover, research and public health purposes, and as required or authorised by law. This process should be more transparent with a better explanation of what it means for both patients and providers.
Removing the need for provider participation agreements seems like a good idea as these documents are very one-sided. But it is not clear to me what this will mean for the liability of organisations, practices and individual practitioners.
A failing strategy
I find it challenging to have a meaningful discussion about incentivising uptake of eHealth when there are so many unknowns. It’s like trying to sell a house that’s still being built and everyone knows there are construction issues. Pushing people to live in the house does not make it a safer or a better building.
The RACGP warns against hastily implementing incentives and advises the department to wait for the outcomes of the Primary Health Care Advisory Group review, the MBS review, and the opt-out trials which are due to start.
Once the identified problems with My Health Record have been addressed and resolved, the RACGP believes that uploading of patient information to My Health Record would be best supported by a practitioner incentive payment (SIP) or an MBS rebate.
It will be interesting to see the response from the department to the criticism. I’m afraid that history will repeat itself: they’ll go full steam ahead, only to discover in one or two years time that the strategy didn’t work. What do you think?