Research published last week has identified the first new human prion disease in 50 years. The paper’s lead author, Stanley Prusiner, who won the Nobel prize in 1997 for his discovery that Creutzfeldt-Jakob disease (CJD) could be transmitted by a “misfolded” protein, says this new disease is also potentially infectious.
Prion diseases are a rare class of brain disorders that are transmissible between animals of any species, including humans. The archetypal such disease is kuru, which spread through cannibalistic rituals in the Eastern Highlands of Papua New Guinea.
Rare and deadly
Kuru affected mostly women and children of the Fore tribe, who ate brains and spinal cords of deceased relatives, and subsequently developed body tremors, balance problems and slurred speech. There’s no cure for kuru and sufferers always died. But it no longer strikes as cannibalism in the region has been eliminated.
Other prion diseases include scrapie in sheep and goats and bovine spongiform encephalopathy (BSE) in cows. When transmitted to humans during the “mad cow disease” outbreak in Europe, BSE resulted in variant CJD (vCJD).
The newly described addition to the prion disease canon, Shy-Drager syndrome (SDS) or multiple system atrophy (MSA), was first recognised in the early 1960s and has many features in common with Parkinson’s disease.
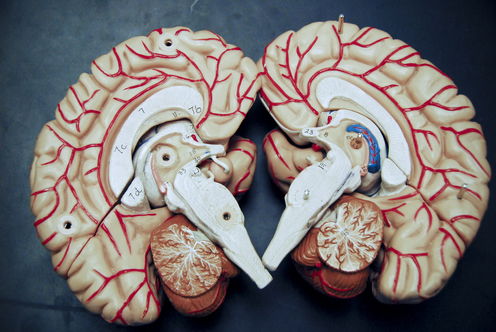
The most important of these is that a protein known as α-synuclein (α-syn) accumulates in the brain, in both Parkinson’s and SDS/MSA. This accumulation is very similar to what happens in CJD, where the prion protein (PrP) accumulates, and also in Alzheimer’s disease and other dementias, where two types of proteins, known as amyloid beta (Aβ-amyloid) and tau, build up in the brain.

The clumps and tangles of these various aggregated proteins cause neurons to degenerate and die. This is a cumulative process which takes between months and decades to manifest as overt disease.
In fact, many of the neurodegenerative diseases of the ageing brain are associated with the accumulation and deposition of specific proteins. It has long been suspected that neurodegenerative diseases in general may all ultimately be caused by this process of proteins getting caught in the wrong process, and misfolding.
This misfolding sets off a cascade of events: the proteins oligomerise (a number of identical molecules join together); accumulate; nucleate (form a nucleus or centre); polymerise (combine to build a structure with its components); self-replicate; and eventually, propagate and spread throughout the brain. Many of these protein changes also occur in the usual food cooking process (aggregation of proteins caused by heating) or food preparation (the solidification of proteins in the refrigerator).
Finally, some but not all of these misfolded proteins gain the ability to be transmitted between people and animals. In fact, the word “prion” was coined by Prusiner in 1992 to describe this property of a pro_teinaceous in_fectious particle. And we don’t yet know of ways to easily “dis-infect” or kill these proteins. All kinds of chemicals that kill bacteria and viruses do not harm prions.
Infectious proteins
Scientists have always kept – and still do – an open mind about whether Alzheimer’s disease and other neurodegenerative conditions are transmissible. We’ve known since the early 1960s that amyloid fibrils – the accumulations of Aβ-amyloid in the brain – are self-propagating entities.
In diseases involving amyloid protein, the “amyloid enhancing factor”, which causes the disease to progress, is thought to be amyloid itself. In other words, the amyloid is self-replicating and makes copies of itself exponentially.

We know that the Alzheimer’s disease-causing human Aβ-amyloid can cross-seed Aβ-amyloid accumulation in genetically susceptible rodents. Mice carrying an unstable and genetically modified human protein can then be “infected” by giving them a dose of the human abnormal protein. But there’s still no direct evidence that Alzheimer’s disease is transmissible between people.
Working out whether SDS/MSA is transmissible, at least from humans to genetically susceptible transgenic cell and rodents, is the first step in testing if it’s transmissible from humans to primates, or indeed among people.
As a precautionary measure, the authors of the paper warn we should now take additional safety precautions in the neurosurgical clinics where deep brain stimulation is used to control the tremors caused by Parkinson’s disease. Because of the overlap in symptoms and signs of Parkinson’s with SDS/MSA, it’s likely that some people with the newly described disease have been treated by deep brain stimulation.
It’s important to ensure that cross-contamination of neurosurgical equipment doesn’t occur because we don’t want to inadvertently transmit a disease between humans. Using disposable stimulation electrodes, for instance, will be mandatory in the future. Similar concerns have already been raised about other neurodegenerative illnesses, such as diseases involving misfolded tau protein, which cause frontotemporal dementia.
With the publication of this paper, the spectrum of prion diseases has been enlarged, perhaps considerably. But until it becomes possible to evaluate the role of intra-species transmission, SDS/MSA will have to remain in the category of “hypothetically transmissible to a genetically susceptible recipient”.
It’s premature to classify it as being the same as CJD, which is clearly transmissible within and between species. That has been made apparent by the mad cow saga, which still has years to run due to the long latency from prion infection to overt disease.
Colin Masters does not work for, consult, own shares in or receive funding from any company or organization that would benefit from this article, and has disclosed no relevant affiliations beyond the academic appointment above.