But demand for donor sperm continues to outstrip supply, prompting clinics to launch recruitment drives or import frozen vials from overseas sperm banks.
Experts estimate about 60,000 people have been born as a result of sperm donations in Australia, where assisted reproduction is regulated but laws vary from state to state.
Here are five things you need to know about sperm donation.
Who can donate sperm?
Donors must produce good quality semen and have no evidence of any hereditary illness or sexually transmissible disease.
Victorian Assisted Reproductive Treatment Authority (VARTA) chief executive Louise Johnson said men who donated sperm were not paid and did so “thoughtfully”.
“The donors have formed their families and appreciate the significance that children bring to people’s lives, or they know somebody who is experiencing difficulties in conceiving and they want to help,” she told the ABC.
Ms Johnson said most Victorian clinics used sperm donors aged between 25 and 45 years old.
“Forty-five tends to be the age the clinics use as a policy cut-off. If you use an older sperm donor there is an increased risk of more DNA mutations in the sperm,” she said.
“Children born from older fathers are also at a slightly greater risk of inheriting a range or disorders including autism and some mental health problems.”
Regulations and protections
Donor insemination has in the past been based on the principle of anonymity.
The Australian Institute of Family Studies said legislation and donor conception practices in Australia have “evolved significantly to encourage greater knowledge and openness”.
There are central sperm donor registries in the states of Victoria, New South Wales and Western Australia.
In other areas, the details of sperm donors are kept by clinics as an accreditation requirement.
The identity of a donor is protected until the child becomes an adult and can apply for this information.
Under Australian law, a sperm donor who donates through a fertility or IVF clinic will not be named on the birth certificate.
However, in Victoria, when a donor-conceived person applies as an adult for their birth certificate, they will receive an addendum stating that further information about this birth is available from the Registry of Births, Deaths and Marriages, Ms Johnson said.
A person is not legally excluded from having parental rights or responsibilities if he donates outside the clinic system using artificial insemination.
It is illegal for donors in Australia to take payment for human tissue including sperm and embryos, although they can be reimbursed for travel and medical expenses.
Online sperm donation
Dozens of unregulated websites and online forums also attempt to match sperm donors with recipients, usually for free.
One of the most popular sperm donation websites is the US-based Known Donor Registry, which launched in 2010 and reportedly boasts 16,000 members.
Once a “match” is made online, women and donors choose a method to conceive: by artificial insemination using sperm deposited in a sterile cup or natural insemination involving sexual intercourse.
There has also been a surge in online sperm donations in China, the New Daily website reported, where donors are paid 5,000 yuan (around $1,000) for their sperm.
In July, China-based e-commerce firm Alibaba teamed up with seven sperm banks to launch an online campaign via its special promotion site, Juhuasuan.
Alibaba said the three-day campaign aimed to “raise awareness of sperm banks in China and make it easier for them to reach potential donors”.
The initiative, which reportedly attracted over 22,000 replies in under 48 hours, was a response to the country’s chronic shortage of sperm donations.
Demand versus supply
While Victoria and Western Australia publish data about donor numbers in their respective states, there is no national data available on the total number of donors used in IVF and insemination cycles.
The people needing to access donor sperm include heterosexual couples having difficulty conceiving because of male infertility, single women and women in same-sex relationships keen to start a family.
According to VARTA’s 2014 annual report, the supply of sperm donors in Victoria has fallen by 23 per cent while the use of donor insemination has almost doubled.
Ms Johnson said while Victorian clinics worked hard this year to successfully recruit more sperm donors, more were needed.
“It is a myth that an end to anonymous donation has affected the number of sperm donors,” she said.
“The supply of donors has remained steady when legislation changed.
“When legislation changed in 1995, requiring sperm donors to agree to provide identifying details to offspring when they reach 18, it didn’t reduce the number of donors coming forward.
“But what has happened since the implementation of those and more recent legislative changes is that the number of women and couples wanting to access treatment has increased.”
This is the case across Australia.
To meet the demand, VARTA said, clinics from Queensland, NSW, the ACT and Tasmania are importing donor sperm from the United States.
Victorian clinics are currently engaged with the statutory authority about the potential for a class application to import sperm from US sperm banks, it said.
Health checks, counselling at clinics
Dr David Wilkinson, fertility specialist at the City Fertility Centre in Melbourne, said going through an accredited clinic was more expensive but offered better protections for the mother and child.
“We do genetic screening, hormonal tests, assisted fibrosis, a whole lot of things which are quite expensive … but I guess the benefits are that it is a lot safer,” he told the ABC.
“And because we are carefully timing ovulation or we are doing IVF treatment, the chance of a pregnancy is much higher than it would be for just trying naturally.”
Donors in Victoria are given extensive counselling to make sure they “fully understand the ramifications” of their choice before proceeding with the donation, Dr Wilkinson said.
“We make sure as much as we can that the donor … understands what they want out of it,” he said.
“We provide some parameters in terms of the physical appearance of the person, the racial background, educational background, sometimes a bit of a bio, too, in terms of what you know they like in life and things.
“So to a degree you know what you are getting. We go to considerable steps to make sure that everything is done by the letter of the law.”
He said Victorian clinics as well as those in South Australia could use one donor for up to 10 families.
In New South Wales, maximum number of births from a single donor is five.
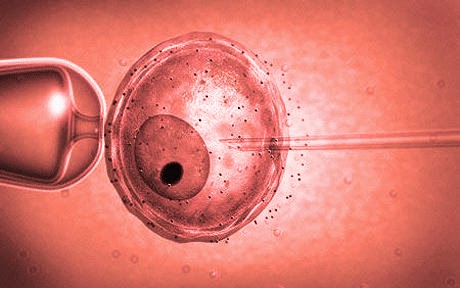
A donor’s sperm are cryopreserved in liquid nitrogen and stored for use in a treatment cycle.
“Routinely we keep it for 10 years — we can extend that with application,” Dr Wilkinson said.
“When we come to use the sperm it is thawed and we can use the sperm for its intended purpose. Either donor insemination or sometimes we use it in IVF treatment.”