When you have a urinary tract infection, something feels very, very wrong down there. There’s a burning or stinging sensation when you pee, dull aching in your lower back, and in some cases you may be urinating blood.
If you’re a woman, odds are you’re going to have at least one in your lifetime, and middle-aged women are more likely to get the infection than men by a ratio of 30 to one. There are an estimated 150 million UTI cases around the world, according to the American Urological Association, and they cost about $6 billion to treat.
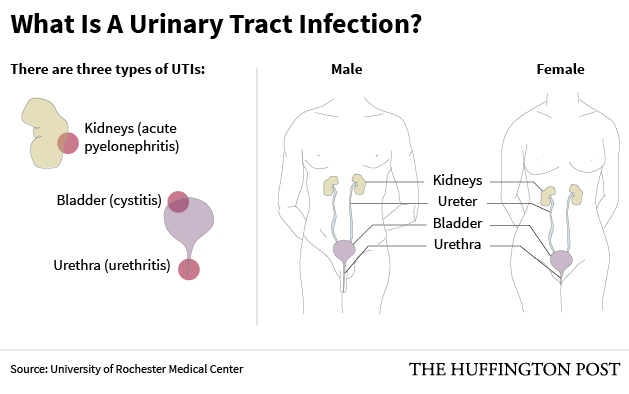
So why are they more common in the fairer sex? It’s simple anatomy. Because of how short our urethras are (the tube that connects the bladder to the outside world,) it’s easier for bad bacteria to enter the body and wreak havoc on the bladder and kidneys. Men, on the other hand, have urethras that extend all the way to the tip of their penises, which gives bacteria a harder road to climb.

Beyond urethra length, there’s another reason women get infections more often than men: The physical act of sex makes it easier for bacteria from the colon to travel to the urethra and find its way into our bodies.
“Sexual intercourse increases trauma to the reproductive tract, [which] makes that damaged tissue more susceptible to invasion by any sort of pathogenic bacteria,” explained Dr. Deborah Wing, an OB/GYN professor at University of California, Irvine. Another way of putting it: “The fun house is so close to the outhouse.”
For obvious reasons, women who engage in anal sex before vaginal sex are more prone to UTIs, and men who perform anal sex without a condom are also at a higher risk of getting bad bacteria all up in their urethras. Diaphragms also increase the risk of UTI, according to WebMD, because they’re often used with spermicide, which can change the bacterial environment of the vagina and bring UTI-causing microbes even closer to the urethra. Repeated antibiotic use is also a factor in UTIs, as they can decimate the body’s natural, protective stores of helpful bacteria, which then allows bad bacteria to gain a foothold. Finally, in post-menopausal women, lower levels of estrogen make it easier for the bacteria to cling to the body.
To treat UTIs, doctors will prescribe one round of antibiotics, which usually clears the infection right up. But in women who get recurrent UTIs (defined as three or more per year), repeatedly downing antibiotics or taking preventive antibiotics after every time you have sex can get a little concerning and in fact may be making the problem worse. Repeated antibiotic use is a good way to wipe out all the helpful bacteria in your body. It’s also a recipe for antibiotic resistance — and there’s evidence that treatment-resistant UTI cases are on the rise. That means doctors are running out of medicines that can defeat some UTIs, including the most common one caused by E. Coli.
If treatment-resistant UTIs become endemic in the U.S., that means more people will suffer from long-term chronic pain, pyelonephritis (when the infection spreads to the kidneys) and bacteremia (when the bacteria spreads to the blood), said Mike Hibbing, a UTI researcher at Washington University in St. Louis. These things can lead to kidney failure and eventually death.
“It’s going to be a major problem as the incidence of antibiotic resistant and multidrug-resistant organisms rise,” he predicted. “Combinations of anti-virulent therapy and preventive measures are going to be essential.”
So what should you do to avoid a UTI? First of all, don’t plan on relying on cranberry juice. While many women swear by this common home remedy, the science is a little murky. A 2012 review of past research showed that women who drank more cranberry juice had fewer UTIs, perhaps because of certain chemicals called proanthocyanidins, which prevent bacteria from clinging to the lining of the urethra and bladder. But clinical trials, which establish if the relationship is causal, have not really found much evidence to support cranberry juice as treatment.
“In a nutshell, none of the clinical trials in non-pregnant individuals seems to demonstrate that there was clinical benefit,” said Wing.
Instead, be proactive and follow these steps to avoid an infection in the first place:

— This feed and its contents are the property of The Huffington Post, and use is subject to our terms. It may be used for personal consumption, but may not be distributed on a website.