Legionnaires’ disease continues to spread in a New York City outbreak that health officials say is the largest and deadliest in the city’s history. The bacterial infection, which causes severe respiratory illness, has now killed eight people and sickened at least 97 since it first emerged in the South Bronx on July 10, the Associated Press reports.
Health officials have linked the ongoing outbreak to a series of cooling towers — the kind buildings use as part of their air conditioning and ventilation systems. Extensive testing revealed that five cooling units in the South Bronx — including at the Opera House Hotel and the Lincoln Medical and Mental Health Center — were contaminated with the bacteria that causes the disease. Legionnaires’ disease can be spread when people inhale water mist from these contaminated towers, but cannot be caught from another person.
The cooling towers have all since been disinfected, but because the disease has an incubation period of up to two weeks, health officials have been expecting more cases to emerge. Dr. Jay Varma, deputy commissioner for disease control at the New York City Department of Health and Mental Hygiene, told The New York Times that the city will be proactively monitoring the cases.
“We expect the case count to rise over the next several days because it reflects what has happened in the past,” Dr. Varma said. “But we are also confident we have done the most intensive, immediate work to cut off any risk, so we anticipate the number of cases will first rise, then fall again.”
With an estimated 8,000 to 18,000 hospitalized cases of Legionnaires’ s time to learn more about this under-recognized disease that’s on the rise nationwide.
Here are ten things you should know:
1. At one point, scientists described Legionnaires’ disease as “the greatest epidemiological puzzle of the century.”
Legionnaires’ disease was first discovered in 1976, in the aftermath of an outbreak that spread among the attendees of an American Legion convention — hence the name. Before long, “dozens of convention-goes were abruptly felled by intense, flu-like symptoms: wracking coughs, painful chills and fevers as high as 107 degrees,” The Washington Post reports. “In the worst cases, victims’ lungs were flooded with a frothy, bloody fluid that filled the spaces between air sacs and prevented oxygen from getting into their bloodstream. The victims with this raging form of pneumonia almost always died.”
Within two weeks of the first case, 20 people had been killed and 115 others hospitalized by the mysterious disease, sparking what scientists called ‘the greatest epidemiological puzzle of the century.”’ It would take public health officials six months to pin down the cause of the infection — a bacteria which they named Legionella pneumophila — but by that time, the disease had killed 34 people and infected more than 221 others.

Media coverage from the first Legionnaires’ disease outbreak in 1976 reveals just how much the mysterious infection was feared.
2. Two different illnesses are caused by Legionella bacteria.
In addition to Legionnaires’ disease, Legionella bacteria can also cause an illness called Pontiac fever. While Legionnaires’ disease presents as a severe form of pneumonia, Pontiac fever is a much milder, influenza-like illness. The two infections do share similar symptoms, including cough, shortness of breath, high fever, muscle aches, and headaches. But unlike Legionnaires’ disease, Pontiac fever goes away without treatment. Scientists say it is not clear why the same pathogen can produce two distinct illnesses.
3. Legionnaires’ disease is hard to diagnose because it shares signs and symptoms with other conditions.
Symptoms of the disease usually begin 2 to 14 days after a person is exposed to the bacteria. Lung infection is common with Legionella because the bacteria thrive in the warm, moist environment of the lungs. Consequently, most Legionnaires’ patients end up developing pneumonia, a condition in which the lungs fill with fluid. Diagnosing the infection requires special laboratory tests, but because the symptoms are not easily distinguishable from other forms of pneumonia, the proper tests are rarely performed; as a result, the disease often goes undetected.
4. Legionnaires’ disease is treatable.
If it’s diagnosed early, Legionnaires’ disease can usually be treated with antibiotics, although patients typically still require hospitalization. The disease is fatal in up to 30 percent of cases, and some people are more likely to become seriously ill after contracting the disease. Those most at risk include people over the age of 50, smokers, and those with chronic lung disease (like COPD or asthma) or weakened immune systems.
5. Legionnaires’ disease is a common cause of severe pneumonia that requires hospitalization.
Eight thousand to 18,000 Americans are hospitalized due to Legionnaires’ disease each year, although many cases go undetected and/or unreported, so the actual number is thought to be significantly higher. In the current outbreak, an alarming 92 out of the 97 people infected with the disease have required hospitalization, showing just how severe the symptoms often are.
 6. Legionnaires’ disease can cause severe complications and death.
6. Legionnaires’ disease can cause severe complications and death.
Respiratory failure, septic shock, and acute kidney failure are all complications associated with the disease. Early treatment with antibiotics is the best line of defense against complications — but since the symptoms can be difficult to pinpoint, delayed diagnosis is common. Complications arising from the disease are often deadly, even for those without weakened immunity: an estimated 10 percent of otherwise healthy people who develop Legionnaires’ disease die due to problems like those mentioned above. The Occupational Safety and Health Administration (OSHA) estimates that the infection kills about 4,000 Americans annually.
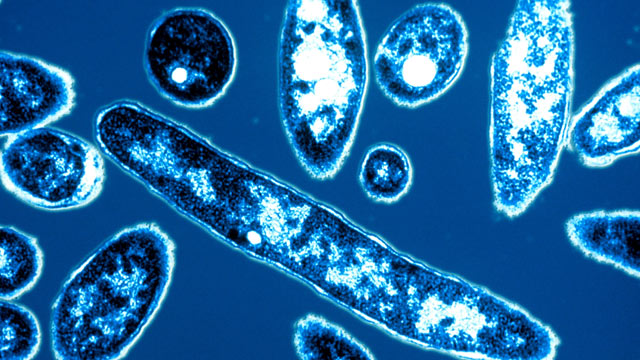
7. Legionella bacteria are usually found in water.
The bacteria occur naturally in the environment, according to the CDC, and they grow best in warm water. Legionella bacteria can multiply quickly in artificial water supply systems like air conditioning systems, and large buildings are more vulnerable to contamination because of their complex water supply systems. Other areas where you might encounter the bacteria include hot tubs and whirlpool spas, hot water tanks, decorative fountains or pools, and large plumbing systems.
8. The disease doesn’t spread from person to person.
Unlike many other infectious diseases, Legionnaires’ disease isn’t spread by insects, animals, or other humans. Instead, the infection is contracted by breathing in mist, steam, or vapor from a water source that has been contaminated with the bacteria, or by aspirating contaminated liquid. Although Legionella bacteria are naturally found in many water sources, they aren’t particularly dangerous until they get into the lungs, which is why we don’t hear about outbreaks associated with drinking water sources. In the case of New York City’s outbreak, many of the infected people are thought to have been simply walking by on the street when they inhaled mist from one of the contaminated cooling towers.

9. Recent travel is a risk factor for Legionnaires’ disease.
More than 20 percent of cases of Legionnaires’ disease may be associated with recent travel. Legionnaires’ disease outbreaks have been linked to hot tubs and whirlpools on cruise ships, swimming pools, and water systems in hotels, hospitals, and nursing homes. Outbreaks of Legionnaires’ disease among travelers can be particularly difficult to detect because of the variable infection rate (i.e., some people with prolonged exposure won’t get sick, while some people who had only passing exposure will get sick), long incubation period, and the dispersal of people from the source of the outbreak.
10. Legionnaires’ disease is preventable.
The most effective way to prevent the infection is to make sure that water systems like cooling towers, spas, and pools are properly maintained and up to current health and safety codes. You can purchase pool test strips to verify that your water is properly maintained: the CDC recommends using the test strips to check for adequate free chlorine (2-4 parts per million [ppm]) or bromine (4-6 ppm) and pH (7.2-7.8) levels. If you’re in shared housing such as a condominium or apartment building, contact the pool operator or landowner immediately if you find improper chlorine, bromine, or pH levels.
New Yorkers who live in proximity to the affected cooling towers should look for symptoms such as coughing, fatigue and confusion.
If you experience any possible symptoms, seek medical help right away.