Bacteria resistant to antibiotics may be deadlier and harder to treat

Antibiotic-resistant bacteria may be tougher superbugs than previously thought: Not only are these bacteria harder to treat, they appear to be “fitter” in general, meaning they survive better in the host and cause more deadly infections, a new study suggests.
The findings go against the prevailing view in medicine that when bacteria acquire resistance to drugs, they become less “fit” in some way, for example, they spread less easily. Although scientists have assumed this is true, evidence supporting this view is limited, the researchers said.
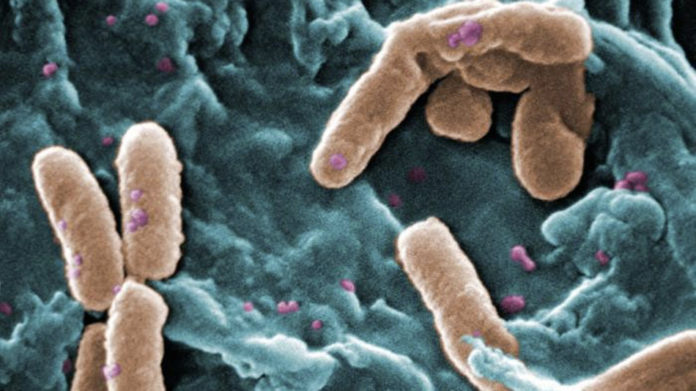
In the new study, the researchers examined the effect of genes on antibiotic resistance in Pseudomonas aeruginosa, bacteria that cause lung infections.
They found that mice infected with antibiotic-resistant strains of P. aeruginosa were more likely to die (without any type of treatment) during the study period than mice infected with P. aeruginosa strains that did not have antibiotic resistance.
The antibiotic-resistant strains were also better able to kill certain immune cells (the body’s defenses against bacteria and other pathogens).
“A potentially overlooked consequence of the acquisition of antimicrobial resistance could be enhanced fitness and virulence of pathogens,” wrote the researchers from Brigham and Women’s Hospital in Boston in the July 22 issue of the journal Science Translational Medicine. The finding “raises a serious concern that drug-resistant strains might be better fit to cause serious, more difficult to treat infections, beyond just the issues raised by the complexity of antibiotic treatment,” they said.
The researchers also had similar findings for two other strains of bacteria: Acinetobacter baumannii, which causes infections in people in hospitals, and Vibrio cholera, which causes the diarrheal disease cholera. For example, V. cholera bacteria with certain genes for antibiotic resistance were better able to grow in the gastrointestinal tracts of rabbits than bacteria without these genes.
“Our results show that efforts to confront the worldwide increase in antibiotic resistance might be exacerbated by fitness advantages that enhance virulence in drug-resistant microbes,” the researchers wrote.
The findings also “emphasize the necessity to effectively control the emergence of antibiotic-resistant pathogens as well as the development of alternative approaches to prevent and treat infections,” they wrote.
Dr. Amesh Adalja, an infectious-disease specialist and a senior associate at the University of Pittsburgh Medical Center’s Center for Health Security, said the new findings were not completely surprising. That’s because mutations that allow bacteria to resist certain antibiotics can have other effects as well, including boosting the bacteria’s ability to survive. “It’s not just a simple trade-off,” between genes for antibiotic resistance and pathogen fitness, said Adalja, who was not involved in the study.
Adalja also noted that researchers have discovered bacteria in caves that are resistant to many antibiotics, even though these bacteria have never had contact with humans, or been exposed to antibiotic drugs. Bacteria likely evolved to have these resistance genes a long time ago, to defend themselves against other bacteria, or help them survive in other ways, Adalja said.
“Antibiotics resistance isn’t just something that happened after the discovery of penicillin,” Adalja said.
The findings show that there may always be some level of antibiotic resistance, even if doctors improve the way they use antibiotics. “There may be limits to what antibiotic stewardship can do,” Adalja said.
This means stopping antibiotic resistance will require more than just judicious use of antibiotics, Adalja said. Researchers need to develop treatments and prevention methods that work in ways that are different from antibiotics, such as drugs that target certain bacterial toxins, or new vaccines, Adalja said.
- Many People Seek Alternative Pain Therapies, But Don’t Tell Doctors
- Alexander the Great’s Father Found — Maybe
- Philip Who? A Gallery of Mystery Bones
- Hearing Aids Meet the Future with Bluetooth Tech
This article originally published at LiveScience here