First-ever 3D human heart simulator may lead to better treatments

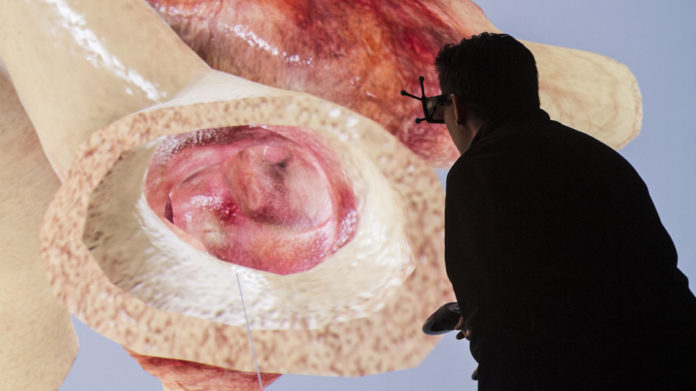
A French company better known for designing aircraft systems announced Wednesday that, on May 29, it will release the world’s first commercially available, scientifically accurate, simulated 3-dimensional (3D) model of a whole, healthy heart.
The model may, with fine-tuning and additional development, help to revolutionize the way that cardiologists match treatments to individual heart patients.
The culmination of the first phase of Dassault Systemes’ “Living Heart Project,” the simulation may soon allow physicians, medical device manufacturers and others to understand disease states and test innovative treatments without resorting to animal testing.
For example, according to Living Heart Project director Steve Levine, it will soon be possible for cardiologists to rehearse difficult procedures using the company’s 3D modeling. Starting on May 29, when the heart model is released, doctors can use the baseline healthy heart to study congenital defects or heart disease by modifying the shape and tissue properties through the use of a software editor.
Levine says that doctors have developed models and simulations of different sections of the heart, but until now, no one had been able to put these pieces together into an holistic simulation.
“What we can now do for devices that go inside the heart is you can test it on the computer the same way you can test planes,” Levine told Mashable in an interview.
The project involves 45 medical professionals, organizations and regulatory agencies, including the Food and Drug Administration (FDA), which oversees the U.S. medical industry. The FDA signed a five-year collaborative research agreement with Dassault to help oversee the development of a heart model that can be used for regulatory science.

The model is powered by Dassault Systemes’ “3DExperience” platform.
An example of how the simulator may be used is in planning for a valve replacement. Because every person’s heart is a different size and shape, there can be negative consequences if doctors choose the wrong size valve as a replacement. Currently, doctors rely on a 2D image of a dynamic, 3D system, which has considerable shortcomings, Levine says.
However, if they could simulate a valve replacement in 3D first, and see how the heart would respond, then it could lessen the likelihood of negative surgical outcomes, Levine says. “The success rate could be improved quite a bit.”
Dr. David Roberts, the chief of cardiology at the North Shore Medical Center in Salem, Massachusetts, who is not affiliated with the Living Heart Project, told Mashable via email that the simulated heart holds considerable promise.
“I see this as a valuable advance for cardiac researchers especially in device development. However, the really exciting development is to be able to use this technology to individualize therapy for a given patient,” he said.
“To date we have not had the ability to simulate how a patient would respond to a given cardiac intervention (pacemaker lead, cardiac valve or stent) prior to the procedure and have it influence the choices we make,” he said.
“This could be a game changer.”
The Living Heart Project is part of a general push toward simulating the behavior of complex systems in the human body, with applicability for a wide variety of medical fields.
With the heart simulation, doctors can store it on a laptop, and then when they want to simulate the actual beating of the heart, they can upload it to a larger computer, server or the cloud. “The computation is done remotely and then results, through an animation, can be delivered back through a laptop,” Levine says.
In addition, the simulation can also be delivered in 3D display environments like Oculus Rift, allowing doctors to go inside patient’s hearts, virtually speaking.
“We’ve built some demonstrations where we’ve built a holographic tablet,” Levine says.
For Levine, this research is personal, as he has a daughter who was born with her ventricles transposed. “They don’t really understand the mechanics of her heart at all,” he said. He hopes the new technology will enable doctors treating cases like hers to develop new insights into congenital heart defects in particular.
Levine says some cardiologists are interested in the device to use it for explaining conditions and procedures to patients, with research showing that more confident patients tend to have better health outcomes.
“I’ve had many cardiologists… really emphasize that we can really help immediately with patients’ confidence and understanding” of what’s happening to them.
In other words, patients may soon take a tour of their own heart before they go under the knife.