Some aspects of Australia’s healthcare system are most visible from the angle of a hospital bed. That was exactly where I was lying when I wrote this, shortly before Joe Hockey cut health spending by a further $2bn in his second attempt at a budget.
I am going through an established procedure for the bone marrow cancer multiple myeloma at Canberra hospital. The hospital is not tottering on the verge of collapse. The workers here are providing vital services but it’s tough for them.
Canberra hospital staff are, in general, very dedicated and capable. They are also very exploited, therefore alienated, by low pay, disagreeable shift work, inadequate working conditions and lack of collective control over what they do. In both respects, Canberra hospital is like all public hospitals in this country.
There aren’t enough beds, either. Nor is there enough money or staff. Some staff would be more effective with more paid training. Overall, it is like other large workplaces: an authoritarian, top-down bureaucracy.
Just after my cancer diagnosis, I was given the option of joining a clinical trial. Clinical trials are an important part of improving the treatment of illnesses. Good trials study the effects on large numbers of volunteer patients of a new procedure compared to established ones. They are funded by hospitals, governments, medical corporations and charities.
Both knowledgeable friends and my doctors pointed out the advantages of signing on for the trial. It’s not a selfless thing to do, though – if you’re on a clinical trial much more attention is paid to you. You’re special, not just an ordinary patient; subject to closer observation, in effect you experience a higher staff to patient ratio; and the details of the treatment are controlled by even more rigorous guidelines than usual.
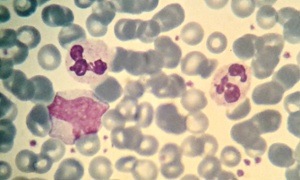
Multiple myeloma crowds out normal blood cells in bone marrow. Its consequences include weak bones, reduced immunity, anaemia and kidney problems. It is incurable but can be significantly slowed down.
I decided to delay treatment because I was told that the point at which I started would not have a significant effect on my life expectancy and I wasn’t feeling too bad. The disease progressed and I decided that it was time to start treatment, before there was major damage to my bones, kidneys and immune system.
By that stage, the clinical trial had closed.
After months of first one, then a second chemotherapy regime, I was ready for an autologous blood stem cell transplant. None of the treatment was physically or mentally pleasant for me and it also stressed people I love and care about.
Millions of my own blood stem cells were filtered out, through an impressive machine – essentially a very sophisticated little centrifuge – under the supervision of highly trained and competent workers.
A few weeks later, I was ready to have half of these put back. That would happen the day after a dose of very poisonous chemotherapy designed to kill off the cancer cells, which would also totally knock out my bone marrow and therefore my capacity to make new blood cells. For a period of several days, I would have no immune system.
Once slipped back into my bloodstream, the previously harvested cells would rebuild my bone marrow. The process of the old bone marrow dying and the new being rebuilt takes weeks and you are pretty crook while it’s happening. The goal: to set the cancer back and give me more years of more comfortable life.
There was a delay between the stem cell harvest and the chemo poisoning and “reinfusion”. A chest x-ray, one of the tests the day before the chemo, showed up something – they weren’t sure what it was. I was put on two additional antibiotics. This x-ray had to be sorted out.
Initially, I was pretty depressed about the delay, having prepared for the heavy stuff of the poison chemo and transplant. But I diverted myself with work.
After more than a week, it turned out that what the x-ray (and a CT scan and another x-ray) showed was not a matter of concern for a group of respiratory specialists who had a look at the images. Then the transplant had to be rescheduled.
More time passed and, well, you might say Easter intervened. The doctors involved are all highly qualified, busy people, not to mention the specialised nursing staff, and beds are expensive. Every day without treatment was a day for the cancer cells in my bone marrow to multiply.
So, while I waited, I was put back on a maintenance dose of the drug that had been most effective in reducing the cancer during the second chemotherapy regime. You may have heard of it: Thalidomide.
Used to treat pregnant women with nausea in the 1950s and 1960s, it was a total disaster, causing severe birth defects. But it can be an effective treatment for myeloma. There are side effects in addition to those for pregnant women. Thalidomide can lead to tiredness, lack of mental sharpness and “peripheral neuropathy” – progressive loss of feeling in fingers, hands, toes and feet. Some of that loss can be permanent.
I experienced these side-effects both during the first and then the Thalidomide chemo regime and they returned when I went back on a lower dose of Thalidomide. I wondered, would this delay have occurred if I was on a clinical trial, meaning that extra money had been invested in my treatment? Probably.
Very early last Friday morning, in my high care room, I made some cancerous reflections on health care. It occurred to me, selfishly, that some of the other problems in my treatment may not have happened if I’d been on a clinical trial either.
Then, I thought, actually, the fundamental issue isn’t participating in a clinical trial. Perhaps for individuals receiving treatment, participating in a trial can make things run more smoothly. But health care shouldn’t be about special advantages for a chosen few.
The length of the delay in my treatment was conditioned by the state of hospital funding and staffing and ultimately the priority that governments give to health. At this moment, our government would rather spend our taxes on locking up refugees, prisons and policing, stupendously expensive “defence” equipment, celebrating wars and special grants for people who argue that climate change is not a big deal.
Their fundamental purpose is ensuring that healthy profits can be made by business. Hence their priority of not upsetting the wealthy or corporations by taxing them too much or, in some cases, at all. So public spending on lower priorities, like health have to be “kept under control”.
Another experience raises the same issue. After the poison chemo and reinfusion I stayed at home, under the amazing care of my partner, and visited the haemotology outpatients clinic daily. But, I was told, I had been admitted to the oncology ward, so that I could get straight into a bed if I was feeling bad and particularly if I caught an infection.
Following five days at home, my neutrophil count was on the on the way down. Neutrophils are a kind of leukocyte blood cell – they combat bacteria and funguses. I was extremely vulnerable to infection, it was time to go into the ward.
A bed had been secured for me five days earlier, I was told. It was free and waiting. But getting into that bed took quite a while. Seven hours in the outpatients clinic and another hour in an oncology ward waiting room. Seven hours when I had already been marked for speedy admission.
For others, waits are much longer. As the government continues to de-prioritise the health and welfare of its citizens, they will get longer still.