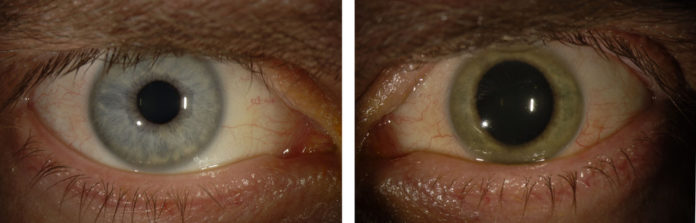
Before he contracted Ebola, Dr. Ian Crozier had two blue eyes. After he was told he was cured of the disease, his left eye turned green. Credit Emory Eye Center
When he was released from Emory University Hospital in October after a long, brutal fight with Ebola that nearly ended his life, Dr. Ian Crozier’s medical team thought he was cured. But less than two months later, he was back at the hospital with fading sight, intense pain and soaring pressure in his left eye.
Test results were chilling: The inside of Dr. Crozier’s eye was teeming with Ebola.
His doctors were amazed. They had considered the possibility that the virus had invaded his eye, but they had not really expected to find it. Months had passed since Dr. Crozier became ill while working in an Ebola treatment ward in Sierra Leone as a volunteer for the World Health Organization. By the time he left Emory, his blood was Ebola-free. Although the virus may persist in semen for months, other body fluids were thought to be clear of it once a patient recovered. Almost nothing was known about the ability of Ebola to lurk inside the eye.
Despite the infection within his eye, Dr. Crozier’s tears and the surface of his eye were virus-free, so he posed no risk to anyone who had casual contact with him.
More than a year after the epidemic in West Africa was recognized, doctors are still learning about the course of the disease and its lingering effects on survivors. Information about the aftermath of Ebola has been limited because past outbreaks were small: no more than a few hundred cases, often with death rates of 50 percent to 80 percent. But now, with at least 10,000 survivors in Guinea, Liberia and Sierra Leone, patterns are emerging.
Dr. Crozier, 44, ruefully calls himself a poster child for “post-Ebola syndrome”: Besides eye trouble, he has had debilitating joint and muscle pain, deep fatigue and hearing loss. Similar problems are being reported in West Africa, but it is not clear how common, severe or persistent they are. There have even been reports of survivors left completely blind or deaf, but these accounts are anecdotal and unconfirmed.

Dr. Crozier’s left eye regained its blue color following treatment. Credit Kevin Liles for The New York Times
Doctors say the eye problems, because they threaten sight, are the most worrisome part of the syndrome and most urgently need attention. Dr. Crozier’s condition, uveitis — a dangerous inflammation inside the eye — has also been diagnosed in West Africans who survived Ebola.
At the height of the epidemic, health workers were too overwhelmed with the sick to worry much about survivors. But as the outbreak wanes, the World Health Organization has begun to gather information to help those who have not fully recovered, said Dr. Daniel Bausch, a senior consultant to the W.H.O. and an infectious-disease specialist at Tulane University. He added that the reports of eye trouble were of particular concern.
“It’s a major thing we need to study and provide support for,” Dr. Bausch said. But there are hardly any ophthalmologists in West Africa, and only they have the skills and equipment to diagnose conditions like uveitis that affect the inner chambers of the eye.
At ELWA Hospital in Monrovia, Liberia, run by the missionary group SIM, Dr. John Fankhauser, the medical director, said chronic pain, headaches and eye trouble were the most common physical problems among the hundred or so people attending a special clinic for Ebola survivors. Some have such severe pain that they find it hard to walk, he said. About 40 percent have eye pain, inflammation, blurred vision and blind spots in their visual fields. Some have uveitis.
Dr. Fankhauser said he hoped that specialists in ophthalmology, rheumatology and rehabilitation medicine would visit.
“If they see enough patients, they can help us with the trends of what they are seeing, and that may help direct some of our therapy in the future, even after the team’s gone,” he said.
In Sierra Leone, the picture is much the same, according to Dr. John S. Schieffelin, a physician from the Tulane University School of Medicine who volunteered there. He said a strong, well-organized survivor group met regularly in Kenema.
“The main problems they’re telling me about are lots of body and joint pains, chronic headaches and women who stopped having menstrual periods, and for some it’s been several months,” Dr. Schieffelin said. “There’s quite a bit of vision problems.”
He added, “I have met one former patient that does appear to be deaf.”
The hearing loss could result from brain inflammation or very low blood pressure for an extended period, both caused by Ebola, Dr. Schieffelin said.
When Dr. Crozier’s eye trouble began, he and the Emory team suspected that Ebola had weakened his immune system and left him vulnerable to some other virus that had invaded his eye, maybe one that would be treatable with an antiviral drug.
So Dr. Steven Yeh, an ophthalmologist, pierced Dr. Crozier’s eye with a hair-thin needle, drew a few drops of fluid from its inner chamber and sent them to the lab. The results came as a shock.

Dr. Crozier’s eyes were examined again on March 27 by Dr. Yeh at Emory Eye Center in Atlanta. Eye troubles are common among Ebola survivors. Credit Kevin Liles for The New York Times
For Dr. Crozier, it was deeply unsettling to learn that he was still occupied by something that seemed alien and malevolent. “It felt almost personal that the virus could be in my eye without me knowing it,” he said.
Uveitis had been reported in some Ebola survivors from previous outbreaks, and a related virus, Marburg, had been recovered from one patient’s eye. But those cases had seemed uncommon.
A report about Dr. Crozier’s eye condition was published on Thursday in The New England Journal of Medicine.
The inside of the eye is mostly shielded from the immune system to prevent inflammation that could damage vision. The barriers are not fully understood, but they include tightly packed cells in minute blood vessels that keep out certain cells and molecules, along with unique biological properties that inhibit the immune system. But this protection, called immune privilege, can sometimes turn the inner eye into a sanctuary for viruses, where they can replicate unchecked. The testes are also immune-privileged, which is why Ebola can persist in semen for months.
Finding Ebola in Dr. Crozier’s eye threw his doctors off balance. Dr. Yeh had worn a protective gown and one pair of gloves but no mask when he drew the fluid. Doctors wear more protective gear when treating patients known to have Ebola. He could not rule out the possibility that he had been infected, so he slept in the guest room at home and avoided touching his infant son for three weeks, the incubation period of the disease.
Another concern was the examining room where Dr. Yeh had taken the fluid sample. As soon as they got the results, he and several Emory colleagues rushed back there, verified that no one else had used the room, and disinfected every surface.
Additional tests showed that Dr. Crozier’s tears and the outer surface of his eye were Ebola-free, so he posed no danger to others. But his case suggests that doctors performing eye surgery on Ebola survivors could be at risk. It is not known how long the virus can persist within the eye.
The big question was whether the doctors could save Dr. Crozier’s sight. They worried about both eyes, because ailments in one eye can sometimes spread to the other. But there was no antiviral drug proven to work against Ebola, and even if there were, there was no precedent for treating an eye full of the virus.
In addition, the severe inflammation suggested that the barriers that normally protect the eye from the immune system had been breached. So what was damaging Dr. Crozier’s eye? The virus, the inflammation or both? They could not be sure.
The usual treatment for inflammation is steroids. But they can make an infection worse.
“What if it unleashed the virus?” Dr. Crozier said. “We were on a tightrope.”
Maybe an experimental antiviral drug would help, the doctors thought.
Though Dr. Crozier was the patient, he was also part of his own medical team, and his focus on the scientific details helped counter his mounting fear that he was going blind.

As he and his physicians struggled to balance treating the inflammation with fighting the infection, his eyesight continued to deteriorate. They tried high doses of a steroid, prednisone. The drug caused mood swings like a teenager’s, ravenous hunger, weight gain, high blood pressure and insomnia. And still his sight worsened. It was like looking through brambles, he said. He reached a point where all he could see was movement when Dr. Yeh waggled his fingers.
He also had significant hearing loss on the same side. “The whole left side of your life is gone,” he said. “It was a very dark and depressing time.”
He spent Christmas in the hospital with his younger brother Mark, who had stayed with him constantly throughout his illness and recovery.
The pressure inside his eye, which had been dangerously elevated, began to drop — too much. The eye became doughy to the touch, as if it were turning to mush.
“The eye felt dead to me,” Dr. Crozier said.
The biggest shock came one morning about 10 days after his symptoms started, when he glanced in the mirror and saw that his eye had actually changed color. His iris, normally bright blue, had turned a vivid green. Rarely, severe viral infections can cause such a color change, and it is usually permanent.
“It was like an assault,” he said. “It was so personal.”
As the days passed with no sign of improvement, Dr. Crozier and the Emory team began to think he had little to lose. Dr. Jay Varkey, an infectious-disease specialist who had handled much of Dr. Crozier’s care, got special permission from the Food and Drug Administration to use an experimental antiviral drug taken in pill form. (The doctors declined to name it, preferring to save that information for future publication in a medical journal.) They were not even sure that the drug would find its way into Dr. Crozier’s eye.
At first, there seemed to be no effect. But one morning a week or so later, Dr. Crozier realized that if he turned his head this way and that, he could find “portals” and “wormholes” through the obstructions in his eye and could see his brother Mark, who was sitting on the end of his bed.
Gradually, over the next few months, his sight returned. Surprisingly, his eye turned blue again. A video shows him excitedly calling out letters on an eye chart as he works his way down to smaller and smaller type, with his brother and the doctors standing by, laughing.
Was it the antiviral drug? He cannot be sure, but he thinks so.
“I think the cure was Ian’s own immune system,” Dr. Varkey said, explaining that he suspected the treatments had reduced Dr. Crozier’s symptoms and helped preserve his sight long enough for his immune system to kick in and clear out the virus — just as supportive care during the worst phase of his initial illness had kept him alive until his natural defenses could take over.
Dr. Crozier believes information from his case may help prevent blindness in Ebola survivors in West Africa. On April 9, he headed to Liberia with Dr. Yeh and several other Emory physicians to see patients who had recovered from Ebola and examine their eyes.
“Maybe we can change the natural history of the disease for survivors,” Dr. Crozier said. “I want to start that conversation.”