Professor Gwendolyn Gilbert of the University of NSW is a leading campaigner in the bid to cut antibiotic use. Photo: Jessica Hromas
The plagues are coming. Despite warnings from the World Health Organisation about the urgent need to preserve the effectiveness of antibiotics by slashing their use, consumption of the life-saving drugs continues to increase.
As doctors report ever-more cases of antibiotic-resistant superbugs, research into alternatives to antibiotics around the world is progressing at speed, seeming at times to take on an almost desperate edge.
But with calls to cut back little heeded, a new strategy is emerging that might have some effect. It involves demolishing two of the most deeply embedded conventions of antibiotic prescription: that a long course is better than a short one, and that a course, once commenced, must be completed.

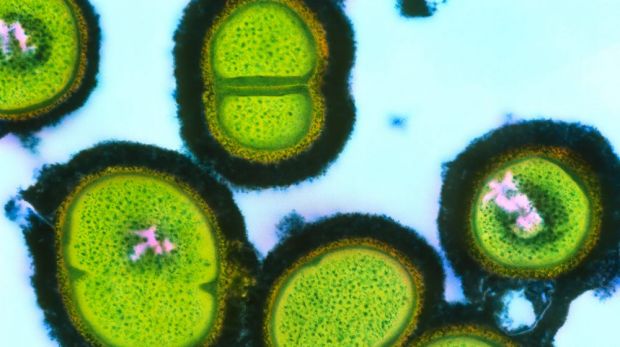
Coloured transmission electron micrograph of a deadly cluster of methicillin-resistant staphylococcus aureus (MRSA) bacteria, which are resistant to antibiotics.
“It’s becoming recognised now that it’s important to monitor a patient’s condition and then stop the antibiotic course when they’ve recovered,” said Professor Gwendolyn Gilbert of the Marie Bashir Institute for Infectious Diseases and Biosecurity at the University of NSW, a leading voice in the campaign to reduce antibiotic use.
“You don’t have to kill every single target bacteria in there, because eventually the body’s immune system will kick in and take over the job. Changing these procedures isn’t easy, but we’re getting to the point where if we don’t do it, we won’t have the antibiotics to treat anyone.”
The danger of antibiotics overuse, universally acknowledged, is that it leads to the development of superbugs – disease-causing bacteria against which drugs have no effect. The best known of these is MRSA?, methicillin-resistant staphylococcus aureus?, which emerged in the early 1960s. Initially restricted to hot-house environments such as hospitals, in the 1990s it started to infect people in the broader community.

A drug-resistant strain of golden staph (ca-MRSA) which can cause serious illness in healthy people.
Since then, many types of resistant bacteria have developed. Indicative is a study conducted by Victorian Healthcare Associated Infection Surveillance System (VICNISS) published in January this year. The study, involving 81 hospitals throughout Australia, looked at surgery-related infections recorded between 2002 and 2013. It found that these cases declined but, at the same time, “antimicrobial-resistant infections increased significantly”. The two most commonly recorded were MRSA? and a super-tough variant of E.coli.
Perhaps because until recently they were perceived as drugs without downsides, and profligate deployment encouraged, data about antibiotic use is surprisingly thin on the ground. Globally, however, the trend seems to be moving relentlessly upwards.
Last year, The Lancet published the results of a Princeton-led analysis of worldwide antibiotic consumption. The study found that, between 2000 and 2010, medical use increased from about 54,000,000,000 “standard units” to 74,000,000,000. China, South Africa, Russia, India and Brazil accounted for three-quarters of the upsurge.

While antibiotics are usually prescribed for five to 14 days, there is no difference in the result when shorter courses are used. Photo: Michel O’Sullivan
Worryingly, the use of hyper-powerful so-called “antibiotics of last resort” increased by 45 per cent during the period.
The figures did not include the use of antibiotics in agriculture, which in the US account for more than 60 per cent of total consumption. A similar percentage pertains in Australia, which imports about 700 tonnes of antibiotics a year, with 550 of those used either as veterinary treatments or agricultural growth-promoters. There are 33 types of antibiotics that are used in both animals and humans – and the question of whether the former affects resistance in the latter remains open.
For the past two years, the independent, not-for-profit Australian pharmaceutical watchdog NPS MedicineWise? has been running a campaign to persuade doctors and patients to reduce antibiotic use. At the start of the campaign, the aim was a 25 per cent cut within five years. Halfway through, NPS MedicineWise? chief executive Dr Lynn Weekes? conceded she was unsure whether the campaign is having any effect.
“The data is mixed,” she said. “It looks like Australia has narrowed the gap between where we were and the OECD average, but it’s not falling fast enough. And the narrowing might actually be because some of the European countries are getting worse.
“The number of people with antibiotic-resistant infections is increasing, and the business model for developing new antibiotics is pretty poor. Antibiotic resistance in Australia is not yet common, but it’s no longer rare.”
In this regard, Australia’s lack of shared borders and its well-developed healthcare system are serving as bulwarks against widespread resistant infections. No one, however, believes these defences will hold for much longer.
University of Queensland microbiologist Dr Patrick Harris has just returned from a year working in Singapore – another high-tech island. He has seen the future – and it has superbugs in it.
“Singapore is very a much a nexus, a bellwether place, with a highly developed healthcare system and the capacity to detect these things,” he said.
“It’s become very clear that in the last few years organisms that are highly antibiotic-resistant are becoming much more common. Five to 10 years ago, cases of antibiotic resistance were vanishingly rare; now they are much more frequent.”
Harris said China, India and Vietnam were all experiencing “a really exponential rise” in infections caused by bacteria that are resistant to all but the strongest broad-spectrum antibiotics.
“In India, if you develop a urinary tract infection there’s a very, very high chance that it will be resistant to first-level antibiotics. And these infections are not just in hospitals, but are now occurring increasingly in the community.”
The picture that emerges at first appears contradictory. It seems nonsensical that when faced with ever-more bugs requiring ever-stronger antibiotics, medical authorities should be suggesting we use fewer of them. The reality, though, lies in the relationship between the two. It is the very ubiquity of antibiotics that is driving evolution of the superbugs.
“Antibiotic use in hospitals is measured as daily doses, over a period of time, and then compared to peer hospitals,” Gilbert explained. “Broadly speaking, the higher the amount of daily doses, the higher the level of antibiotic resistance in the hospital.”
In this respect, the data is clear. Several studies record a broad correlation between antibiotic use and superbug infections in hospitals. Importantly – and key to the thinking of experts in the field – the reverse also applies.
“There is a general rule in hospitals. Excessive use of antibiotics in a hospital will see levels of resistance go up. Remove them, and they go down again,” Harris said.
“To become antibiotic-resistant carries an evolutionary cost. Often, the bacteria will have to fuel a raft of additional mechanisms to maintain that resistance, to keep it all going. If you remove the pressure – the antibiotics – natural selection might make them let these things go, or other ‘wild-card’ variants of the same species of bacteria might out-compete the resistant ones.”
In other words, scaling back the arms race may result in the enemy putting away its weapons.
Given that an across-the-board peace talks seem unlikely, Gilbert sees great scope for achieving a ceasefire by means of thousands of tiny cuts.
“The individual amounts prescribed per case add up to the total amount used,” she said.
“The principle should be to limit the use of antibiotics to an absolute minimum. Often, patients are kept on antibiotics for too long – there is no automatic stop date built in. This is frequently the case in hospitals, but is even more so in long-term care facilities. Elderly patients can be kept on antibiotics – for suspected urinary infections, for instance – with courses just being repeated again and again.
“All these practices increase the likelihood of antibiotic resistance developing. This can happen to an individual patient, but it can then spread to other patients.”
Gilbert said one of the common causes of overuse in hospitals stemmed from their use as “set and forget” drugs of first resort. When a patient presents with an unknown infection, it is standard – and sensible – practice to apply antibiotics as a defence against the development of life-threatening sepsis.
“So doctors tend to err on the side of caution and start treatment quickly, before receiving test results,” she said. “But if the tests come back with a different result to the one expected, then there is a need to discontinue antibiotic use – and doctors need to have the courage to do that.”
Present convention in these situations often finds the doctors continuing the antibiotic treatment on the grounds that it doesn’t do any harm to leave it in place. It is a convention increasingly challenged by an idea called “antimicrobial stewardship”, championed by Gilbert, Harris and Weekes.
The stewardship concept essentially involves the use of third-party assessments of antibiotic use in hospitals. Dispensing habits are checked against patient outcomes in order to identify cases where short courses are just as effective – if not more so – than long ones, and others where pre-emptive antibiotic use can be stopped.
“It’s very difficult to get solid data on this, but there is evidence to suggest that in hospitals where antimicrobial? stewardship is practiced there is a reduction in total antibiotic use,” Gilbert said.
For Harris, the idea has the additional advantage of placing individual antibiotic prescriptions into a community context.
“Doctors always think about their individual patient and not always about the big picture, and that’s where antimicrobial stewardship comes in,” he said. “Antibiotics are a bit different to other medications. When you prescribe them, you’re not just treating your own patient, you’re increasing the risk for everyone else a little bit by potentially boosting resistance down the track.”
A bizarre mix
Recognising the population-wide effect of antibiotics over-use, scientists around the world are conducting a plethora of experiments in the search for alternative ways to kill bacteria.
Work during the past few years has shown, convincingly, that something as simple as using copper instead of stainless steel for bench tops and tap fittings creates a very effective bugicide. Indeed, in March, a chain of supermarkets in Brazil put a copper coating on its shopper trolleys as a public health measure.
Current research represents a bizarre admixture of the ultra-modern and the very old.
At the University of Melbourne, a team is working on infusing silver nanoparticles? into a polymer used to make medical devices such as pacemakers, in order to make them infection-proof.
At the University of Nottingham in Britain, an unprecedented collaboration between microbiologists and ancient historians is testing a 1000-year-old recipe – which included garlic and the bile from a cow’s stomach – found in a medieval? text called Bald’s Leechbook (below) for its surprising ability to treat MRSA.

At James Cook University in Townsville, Queensland, virologists are making viruses attack bacteria found in turtle stomachs. And a company in Colorado has developed a urinary catheter that mimics the structure of shark skin, using micro-patterns to replicate the shark’s ability to prevent bacteria growing on it.
All these approaches may one day soon make an important contribution. But right now, here in Australia, health authorities are gearing up to combat the peak season for antibiotic use – the annual winter cough-and-cold season. The irony of this is well attested, because every single doctor, every single med student, and even most high school kids know that colds are caused by viruses – against which antibiotics are useless.
Nevertheless, in winter many general practitioners prescribe them by the bucketload? – with considerable research suggesting that in many cases they do so simply because they don’t want to dash the expectations of patients who expect to be given pills, even though the pills do no good and the virus will disappear in a couple of days anyway.
“Our research shows that over 50 per cent of doctors have prescribed an antibiotic because a patient asks for it, or expects to be prescribed them,” Weekes said.
“So we try to encourage doctors to suggest other actions, other tools, to help relieve symptoms. One of these is delayed prescriptions – saying antibiotics will be given if the person is not feeling better in 12 or 24 hours. There is some evidence to suggest that in these cases people are less likely to want them when the time comes.”
Harris said it was wrong to deride GPs for prescribing pills that have no effect. Distinguishing between viral and bacterial infections can be tricky, and doctors have a responsibility to be cautious.
“He’s 90 per cent sure it’s a virus, but he’s probably been burned a couple of times before,” he said. “He will employ the precautionary principle, especially if the patient is pressuring him, or says the last time he got sick he ended up in intensive care.
“As doctors, a lot of the time we don’t really know what we’re treating. Most of the time we get it right, but we’re still often wrong. And what happens in GP clinics really is Victorian-level diagnostics: someone looks at the back of your throat and sees some white spots. It’s not a very reliable approach.”
At the University of NSW, Gilbert is also sympathetic but believes it’s time for both doctors and runny-nosed patients to show some courage.
“GPs need to think twice,” she said. “Don’t prescribe antibiotics if you think the cause is viral. And for patients at home, if you’re feeling better, then you don’t have to finish the course.”
There is a distinct urgency to that type of advice, and to campaigns such as the one conducted by NPS MedicineWise?. Antibiotic-resistant superbugs worldwide are increasing in range and in virulence. The first antibiotic, penicillin, was discovered in 1928. It would be a tragedy if the era it engendered came to end after less than a century.
The antibiotic arms race
Antibiotic-resistant superbugs are not new, although their prevalence and severity have increased in line with the wider use of more powerful treatments.
In 1937, sulfonamides – technically not true antibiotics but pretty good at banging bacteria on the head nevertheless – were introduced. Cases of sulfonamide resistance were reported by the end of the decade.
The first true antibiotic was penicillin, discovered in 1928. It was used extensively to treat soldiers during World War II but not made available to the public until 1945 – by which time at least one strain of resistant staphylococcus was in circulation.
And thus the race was on. Tetracycline (1950) was outfoxed by a resistant strain of the gastro-bug shigella? in 1959. Erythromycin (1953) was finally beaten by a form of streptococcus in 1968.
Methicillin? was introduced in 1960, and bested only two years later by a form of staph – the infamous MRSA.
The US Centres for Disease Control lists 11 broad classes of antibiotic in use, and 17 species of bacteria resistant to some or all of them. The super-powerful ceftaroline? class was introduced in 2010. A resistant strain of staph emerged only a year later.
In January this year, a team led by researchers from US firm NovoBiotic? Pharmaceuticals announced the discovery of a new antibiotic, which they dubbed teixobactin?. Writing in Nature, the team reported that in tests the new drug killed bacteria but did not induce the development of resistant strains.
If that remains the case, it will be very exciting. But the 70-year arms race between bugs and antibiotics suggest that only the brave or the foolhardy would be making any bets