A drug-resistant strain of a severe intestinal bug is spreading more rapidly through the population and causing outbreaks in the United States — and it’s put federal officials on high alert.
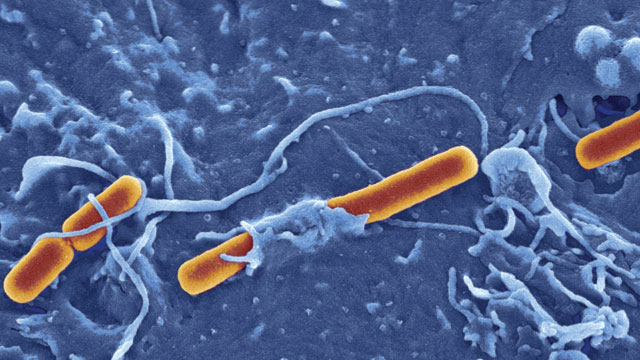
The bacteria, called Shigella sonnei, is one of the germs that causes shigellosis — otherwise known as “Delhi belly” or “Montezuma’s revenge.” Many international travelers are all-t00-familiar with the resulting stomach cramps, diarrhea and nausea that can ruin a vacation or business trip.
Infections caused by Shigella bacteria were once easy to treat with antibiotics. Now, though, the Centers for Disease Control and Prevention is warning that a mutant form of the bug is not only being carried into the U.S. by travelers, but it’s spreading once it’s here.
“This is the first time we’ve documented this large an outbreak of antibiotic-resistant (shigella) linked to international travel,” said the CDC’s Dr. Anna Bowen. “It’s moving itself around the country.”
According to a new report released by the CDC, a strain of Shigella that is resistant to the antibiotic ciprofloxacin (Cipro) infected 243 people in 32 states and Puerto Rico between May 2014 and February 2015. Studies conducted by CDC scientists found that the drug-resistant illness was being repeatedly introduced as ill travelers returned and was then infecting other people in a series of outbreaks around the country.
CDC epidemiologists and local health officials tested cases in Massachusetts, California and Pennsylvania and found that nearly 90 percent of the patients were infected with bacteria resistant to ciprofloxacin (Cipro), which usually is the first drug tried against shigellosis. Before last year, Cipro resistance was found in just 2 percent of Shigella infections tested in the US.
That’s particularly bad news because most Shigella in the U.S. is already resistant to the antibiotics ampicillin and trimethoprim/sulfamethoxazole. This leaves doctors with fewer choices for treating the infections.
Shigella, considered far more serious than other intestinal bugs such as Salmonella or e.Coli, causes about 500,000 cases of diarrhea in the U.S. every year, CDC says. Most cases go away without any need for treatment. But it’s important to have the option to use antibiotics, especially for severe cases and people whose immune systems are compromised, like HIV or cancer patients.
The CDC and the White House, joined by international health agencies, have been sounding the alarm recently about the rise of antibiotic-resistant superbugs. This adds another one to the mix.
“These outbreaks show a troubling trend in Shigella infections in the United States,” CDC director Dr. Tom Frieden, M.D., M.P.H., said in a statement. “Drug-resistant infections are harder to treat and because Shigella spreads so easily between people, the potential for more – and larger – outbreaks is a real concern.”
Like most stomach bugs, Shigella is spread when people get it on their hands and then touch their mouths or noses. It’s one of the main reasons people are urged to wash their hands when using restrooms and especially when handling food.
“Shigellosis can spread very quickly in groups like children in childcare facilities, homeless people and gay and bisexual men, as occurred in these outbreaks,” the CDC says.
“The increase in drug-resistant Shigella makes it even more critical to prevent shigellosis from spreading,” said Dr. Anna Bowen, a medical officer in CDC’s Waterborne Diseases Prevention Branch who led the study. “Washing your hands with soap and water is important for everyone. Also, international travelers can protect themselves by choosing hot foods and drinking only from sealed containers.”
About half of patients whose details were known had links with international travel, mostly to the Dominican Republic and India, the CDC report said. In a San Francisco outbreak that sickened 95 people, half the victims were either homeless or living in single-room occupancy hotels.
Drug resistance, which occurs when bacteria acquire genetic changes that give them the ability to withstand antibiotics, accounts for about 700,000 deaths around the world each year. The World Health Organization said last year that bacteria resistant to antibiotics have spread to every part of the world, and if left unchecked, will take us back to a “pre-antibiotic era” in which minor infections like strep throat could kill. By 2050, scientists predict that drug-resistant bacteria could kill as many as 10 million people annually.