The progressive wasting of muscle and fat tissue throughout the body is one of the most visible and heartbreaking manifestations of cancer, yet little is known about how tumors cause distant tissues to degenerate. Two independent studies published April 6 in Developmental Cell reveal that a tumor-secreted molecule called ImpL2 drives the loss of fat and muscle tissue in fly cancer models that replicate key features of tumor-induced wasting in humans. The findings could lead to the development of much-needed targeted therapies for wasting syndrome in cancer patients.
“Many cancer patients die not because of the local effects of tumors, but rather from more broad, systemic changes to the entire body that are induced by these tumors. One of the worst of these long-range effects is wasting syndrome, also known as cachexia, which is a major obstacle to cancer treatment,” says developmental biologist David Bilder of the University of California, Berkeley, one of the study authors. “The two new studies illustrate the power of using simple model organisms to provide new insights relevant to the most important questions of human cancer biology.”
About 20% of cancer deaths are due to cachexia, which mostly affects patients with advanced cancer, making them too weak for some types of chemotherapy and radiation therapy and more susceptible to the toxic effects of chemotherapy. An increase in food intake does not fully reverse tissue loss, and available therapies are so limited that the National Cancer Institute highlighted cachexia as a perplexing problem that has slowed progress against cancer.
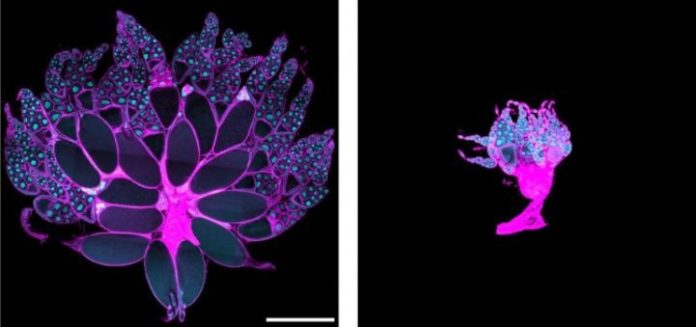
To tackle the complexities of cancer cachexia, two independent research teams– one consisting of Bilder and Alejandra Figueroa-Clarevega of UC Berkeley and the other including Norbert Perrimon of Harvard Medical School and his collaborators–exploited powerful genetic approaches in the fruit fly to rapidly identify the factor responsible for cachexia-like wasting. While Bilder’s team induced cancer in flies by transplanting tumors into the abdomen, Perrimon and his collaborators activated a protein called Yorkie to induce tumorous cell proliferation in intestinal stem cells.
In both of these cancer models, the two teams discovered that a tumor-secreted molecule called ImpL2 caused the wasting of fat, muscles, and ovaries–organs that store energy in the form of lipids and proteins in the fruit fly. ImpL2 is the fly version of mammalian insulin growth factor binding proteins (IGFBPs), which inhibit the activity of a hormone called insulin, thereby interfering with the absorption of glucose from the blood to skeletal muscles and fat tissue. The researchers found that depletion of ImpL2 levels, either specifically in malignant tumors or in abnormally proliferating intestinal stem cells, significantly reduced wasting in the flies.
“Because humans have several homologous IGFBPs, the studies suggest new candidates for mediators of cachexia, which could point to novel therapeutic approaches,” Bilder says. “If specific IGFBPs could be identified that mediate cachexia from certain tumor types, then blocking those proteins could offer a more targeted and effective approach than systemically administering insulin, which risks stimulating tumor growth.”
An intriguing question arising from the studies is how growing tumors evade the effects of ImpL2, even though the molecule causes other tissues to degenerate. One clue uncovered by Perrimon and his collaborators was a disparity in insulin signaling and glucose metabolism between the gut and distant tissues. Proliferating intestinal stem cells showed increased insulin signaling and higher levels of enzymes that break down sugar for energy, when compared with muscles and ovaries.
“The findings suggest that the proliferating tumor cells consume a lion’s share of glucose for energy, while the rest of the body progressively starves,” says Young Kwon of Harvard Medical School, the lead author on the second study.
Because ImpL2 depletion did not fully reverse tissue loss, the research teams will next look for additional factors that influence cancer wasting in flies. “The fruit fly models will enable genome-wide forward genetic screening to identify novel genes that regulate the wasting process,” Kwon says. “The existing mammalian models of wasting are not really suitable for such a screen due to the high cost. Therefore, the fly models will provide a unique opportunity to identify previously unexplored targets for the treatment of wasting syndrome in humans.”
Story Source:
The above story is based on materials provided by Cell Press. Note: Materials may be edited for content and length.
Journal Reference:
- Alejandra Figueroa-Clarevega, David Bilder. Malignant Drosophila Tumors Interrupt Insulin Signaling to Induce Cachexia-like Wasting. Developmental Cell, 2015; 33 (1): 47 DOI: 10.1016/j.devcel.2015.03.001