A Singapore led study has shown that Hepatitis B Virus Infection (HBV) exposure increases the immune system maturation of infants, which may give a better survival advantage to counteract bacterial infection during early life. These findings radically modify the way that HBV vertical infection of neonates (mother-to-child) is portrayed, and present a paradigm shift in the approach to treatment of patients with chronic hepatitis B.
The research, published in Nature Communications on 25 March 2015, was led by Professor Antonio Bertoletti from the Emerging Infectious Diseases Program (EID) at Duke-NUS Graduate Medical School (Duke-NUS).
Currently widespread in Asia, HBV affects approximately 300 million people worldwide while 6 in 100 Singaporeans are chronic carriers. The majority of HBV chronic infections in Asia are acquired at birth. While there is a safe and effective vaccine available, 5% to 10% of babies born to HBV positive mothers still contract the infection. Conventionally, HBV is thought to exploit the immaturity of the neonatal immune system to establish persistent infection.
Current guidelines from international liver associations recommend treatment for HBV carriers only when they show clear signs of active liver disease, typically after the age of 30. This is based on the assumptions that HBV is considered harmless until symptoms of the disease emerge, and that young patients are immune-tolerant to HBV, meaning they have no protective response to the virus and are unable to react to treatment.
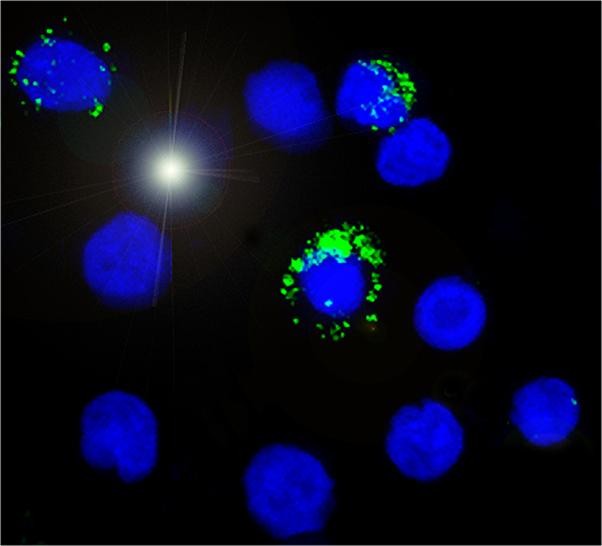
Prof Bertoletti, in collaboration with the National University Hospital (Singapore) and Universitaria di Parma (Italy), showed that contrary to current belief, infants exposed to HBV are not immune-tolerant but they have more mature immune systems. The team examined the immune cells in the cord blood of mothers who were HBV positive and discovered that both the innate and adaptive immune cells are more activated and mature, and they respond better to bacteria challenge, a phenomenon called “trained immunity.” These suggest that their immune cells may be more acclimatised to dealing with potential bacterial infections than the cells from cord blood of healthy mothers.
First author, Duke-NUS Research Fellow Michelle Hong, is heartened about contributing to the understanding of a disease that is endemic in Asia. “Our work contributes to the understanding of how HBV exposure before birth shapes the global immune response of newborn infants and transforms the way we look at HBV. Despite causing diseases later in life, HBV might actually be beneficial to humans early in life.”
Previously, Prof Bertoletti had shown that young adults (aged 14 to 30) with chronic HBV infection are not immune tolerant and possess immune cells able to counter the virus. Moving forward, he plans to examine the impact of HBV infection in paediatric patients; those aged two to 12, to determine how their immune system responds to the virus. The combined findings from these different studies are poised to shape the guidelines for chronic HBV treatment in patients — starting from young adults’ or even earlier.
Story Source:
The above story is based on materials provided by Duke-NUS Graduate Medical School Singapore. Note: Materials may be edited for content and length.
Journal Reference:
- Michelle Hong, Elena Sandalova, Diana Low, Adam J. Gehring, Stefania Fieni, Barbara Amadei, Simonetta Urbani, Yap-Seng Chong, Ernesto Guccione & Antonio Bertoletti. Trained immunity in newborn infants of HBV-infected mothers. Nature Communications, March 2015 DOI: 10.1038/ncomms7588