Chronic disease accounts for 7 of every 10 deaths in the United States and more than 75% of total health care costs. Among people 65 years old and older, over 92% suffer from one or more chronic diseases. By 2020, it is estimated that 48% of the total population will have chronic disease. In an article published in The American Journal of Medicine, researchers discuss how existing health care delivery models are poorly constructed to manage chronic disease, and how a reengineering of the health care system might offer some hope in meeting this challenge.
“Chronic disease has become the great epidemic of our time,” comment authors Richard V. Milani, MD, Ochsner Clinical School — University of Queensland School of Medicine, New Orleans, LA, and Carl J. Lavie, MD, Ochsner Clinical School — University of Queensland School of Medicine, and Louisiana State University System, Baton Rouge, LA. “Our current delivery model is poorly constructed to manage chronic disease, as evidenced by low adherence to quality indicators and poor control of treatable conditions. New technologies have emerged that can engage patients and offer additional modalities in the treatment of chronic disease. Modifying our delivery model to include team-based care in concert with patient-centered technologies offers great promise in managing the chronic disease epidemic.”
According to Milani and Lavie there are four factors that negatively impact the delivery of chronic disease care in the U.S.: physician time demands, rapidly expanding medical database, therapeutic inertia, and lack of supporting infrastructure.
The current U.S. model for delivery of chronic disease care rests with the primary care physician. The authors note that with a median length of a physician visit of less than 15 minutes, there is little time to address the root causes of many chronic diseases, such as poor nutrition and physical inactivity. Even when lifestyle modification advice is provided by the physician, patient adherence rates are disappointingly low.
The second factor that compromises chronic disease care is the incredible growth in medical literature, with 1.8-1.9 million articles published every year. The ability to keep up-to-date with accepted medical evidence is nearly impossible for a busy physician. This is further affected when a significant percentage of studies contradict current medical practice, adding to the burden.
Therapeutic inertia, the third factor, describes a situation in which a provider fails to modify a therapy when the original treatment goals remain unmet. For example, failure to intensify therapy in hypertensive patients with blood pressure greater than 140/90 has been reported to be as high as 86.9% of visits. The clinician, the patient, and the health care system all play a contributory role in this factor.
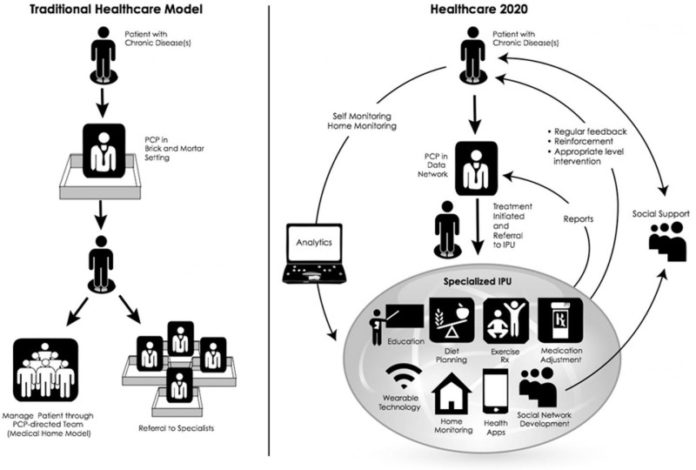
The fourth factor is the care model supporting the patient and physician. Studies have consistently shown that providing the primary care physician with a team-based infrastructure of specialized, non-physician caregivers whose role is to provide a continuous framework of monitoring and management, improves adherence to quality measures and yields superior outcomes, cost, and patient satisfaction.
Milani and Lavie describe specialized integrated practice units (IPUs), each employing nonphysician personnel such as pharmacists, advanced practice clinicians, nurses, health educators, dietitians, social workers, counselors, and therapists, all organized around the patient’s medical condition.
The authors also note that social network influences have had considerable positive impact on behaviors associated with smoking, diet, exercise, depression, medication adherence, and obesity and successful disease management strategies that utilize the potential of social networks may provide sustainable and cost-effective solutions for patients with chronic diseases.
“Today, health care must reengineer its care delivery model to manage the chief medical crisis of the 21st century, chronic disease. The capacity of the stand-alone physician to produce high-quality, evidenced-based care, yielding meaningful and lasting change in lifestyle behaviors, has proven elusive. A new model of team-based care organized as an IPU will have the ability to deliver comprehensive consistent treatment and advice using a focused-factory approach. The IPU will employ the latest in technology innovation, thus better engaging patients, in addition to providing high-quality, consistent, personalized care delivery, and accelerate consequential lifestyle change,” explain Milani and Lavie.
Story Source:
The above story is based on materials provided by Elsevier. Note: Materials may be edited for content and length.
Journal Reference:
- Richard V. Milani, Carl J. Lavie. Healthcare 2020: Reengineering Healthcare Delivery to Combat Chronic Disease. The American Journal of Medicine, 2014; DOI: 10.1016/j.amjmed.2014.10.047