Bacteria that talk to one another and organize themselves into biofilms are more resistant to antibiotics. Researchers are now working to develop drugs that prevent bacteria from communicating.
The aim is to find alternatives to antibiotics and reduce the number of antibiotic-resistant bacteria.
“Understanding how bacteria communicate could provide a new means of controlling them and preventing and treating infectious diseases,” says Professor Anne Aamdal Scheie at the Department of Oral Biology at the University of Oslo.
Together with Professor Fernanda Cristina Petersen, Aamdal Scheie is shedding light on one of the most important health challenges facing the world today, namely antibiotic resistance. The researchers believe that understanding bacterial communication has a key role to play in the fight against resistant bacteria.
Organized bacteria
About 80 percent of our infectious diseases are caused by bacteria organized into biofilms.
“Biofilms are found almost everywhere. They are a kind of society in which millions of bacteria work together. Biofilms form easily wherever there are bacteria, moisture and a few nutrients, such as in the mouth, in the intestines, on the skin, on ships, oil rigs, and in machinery and pipes,” says Aamdal Scheie.
In good biofilms, such as those on the skin, in the mouth or in the intestines, the bacteria protect us from dangerous intruders.
“We have ten times as many bacterial cells as ordinary cells in our bodies, and we are completely dependent on them to be able to function, but we need them to be in balance. A biofilm that forms in the wrong place, such as in an organ, on an implant or in a wound, can spell trouble. If undesirable bacteria are able to evolve, the situation can become dangerous,” says PhD student Ingun Lund Witsø, who works on E. coli bacteria.
More resistant
To form a biofilm, bacteria communicate using various signalling molecules. Within the biofilm, they acquire new properties. They communicate more effectively with one another and exchange information more quickly. In addition, they can switch on and off genes that make them harmful.
“These properties make the bacteria more resistant to antibiotics and to the host’s immune response. Certain antibiotics can penetrate biofilms, but their efficacy is usually greatly reduced. We generally need to increase the concentration of an antibiotic 10-1,000 times to get an effect equivalent to that seen in free-floating bacteria,” says Aamdal Scheie.
Research groups at the Faculty of Dentistry therefore want to understand how bacteria talk to one another — precisely to prevent them from communicating and becoming hazardous.
Disrupts communication
In collaboration with Professor Tore Benneche at the Department of Chemistry, the researchers are examining chemical substances that they believe can inhibit or disrupt communication in bacteria. They are particularly interested in a substance called thiophenone.
“Thiophenones are sister molecules of furanones, which are produced by particular marine red algae and which prevent the algae from becoming coated in bacteria. We have replaced an oxygen molecule with a sulphur molecule to create a more potent drug. Our synthetic thiophenones seem able to inhibit a number of bacteria, including E. coli, which is found in the intestines of animals and humans and which can cause disease,” says Aamdal Scheie.
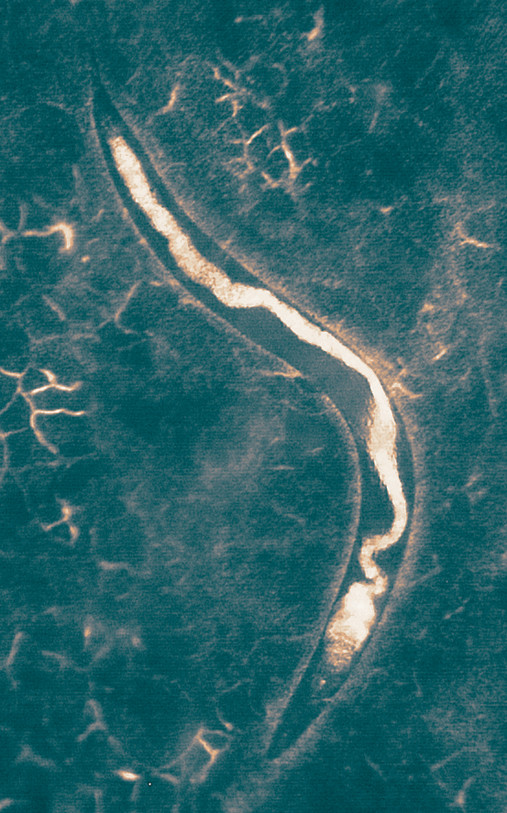
The researchers are testing the new group of drugs in transparent worms called C. elegans, in which they can trace the bacteria while infection develops. They do this by feeding the worms with fluorescent bacteria.
“We feed harmful bacteria into the worm’s body to induce infection. Then, when we supply the worms with thiophenone, we see that the number of bacteria in the stomach and intestines of the worms decreases. A greater number of the worms survive, and they live longer than those not given thiophenone,” says Ali-Oddin Naemi, who is head engineer in Aamdal Scheie’s research group.
Some of the drugs affect the microorganisms’ ability to form communities. Biofilms become smaller with the use of thiophenone, and genes that contribute to disease are also switched off. Thus thiophenones do not kill the bacteria, as antibiotics do, but instead render them harmless. This means that selection pressure is not applied, and so there is little risk of developing resistance to thiophenones.
“It will be some time before these drugs can potentially be used in humans. Nevertheless, the aim is for thiophenone to be able to replace antibiotics, to work in combination with them or, in some cases, to restore the normal bacterial flora,” says Aamdal Scheie.
Editing the DNA
Every year, 25,000 Europeans die from diseases caused by antibiotic-resistant bacteria. Indeed, the World Health Organization believes that current antibiotic usage is the greatest threat facing public health. Norway has been good at keeping antibiotic usage relatively low and has long had a low prevalence of resistant bacteria. However, in a recent doctoral thesis, medic and researcher Jon Birger Haug shows that there has been a marked increase in the use of antibiotics in Norwegian hospitals.
“If we get to the stage where we no longer have antibiotics that work, there will be many types of treatments that we will not be able to perform. Even the simplest operations could become impossible,” Petersen says.
While Professor Aamdal Scheie’s group have shown that they can influence bacterial communication with thiophenones, Petersen and her group are studying how communication occurs in bacteria by editing the bacteria’s DNA.
“In the lab we are trying to crack the code used by the bacteria and work out how they communicate with one another. We are focusing in particular on streptococcus, which accounts for around 40 per cent of the bacteria inside our mouths. By editing bacterial DNA, we can study the effects of signalling molecules and discover new functions. Each new signal can open up novel ways of fighting infections. Part of the battle will also be to recruit good bacteria in the fight against the disease-causing ones. The ultimate goal is to understand the bacteria’s ability to communicate and collaborate so that we can use this knowledge to disarm them,” says Petersen.
Story Source:
The above story is based on materials provided by University of Oslo. Note: Materials may be edited for content and length.