Chicago Bulls guard Derrick Rose is to have knee surgery to repair a torn medial meniscus in his right knee. While I am not privy to the details of his injury and cannot comment on his procedure, what I can tell you is that there is no such thing as a “standard procedure” when it comes to meniscus surgery.

All too often I hear, “I was told I have a torn meniscus cartilage in my knee. The doctor said it is a standard procedure to just remove the torn part. He does it all the time.”
“Ugh,” I think. Actually, each person is different. Each knee is different. Each torn meniscus cartilage is different. And most importantly, the outcome of each procedure is different.
Here’s why.
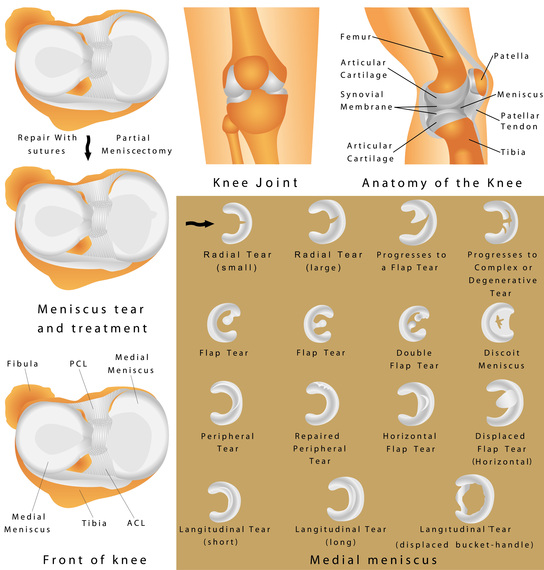
The meniscus is the key shock absorber in the knee. When even small amounts of it are removed, the force concentration on the tibia goes up, wearing away the bearing surface and leading to early arthritis. When torn, the goal is to save as much of the meniscus as possible, preferably by repairing it or, if its truly irreparable, by removing as little as necessary to recreate a smooth surface from the frayed edges. Even the most common tears often have extra side tears or hidden degenerative areas that can affect the results.
The artistry of the surgeon determines how smooth and shaped the remaining tissue is. The scientific understanding of the surgeon to how important the tissue is, how to stimulate a new blood supply, how to use stem cells and growth factors to augment healing, how to suture the torn edges, or if necessary how to replace the meniscus with a new donor meniscus, all pre-determine how the surgeon is going to act when faced with the unique tear inside your knee.
You always need to know the bias of your surgeon. How often does he or she suture torn meniscus cartilages? Do they know how much to save in order to be able to replace the missing tissue successfully? Or is your surgeon a total joint replacement fan who thinks removing the torn tissue is no big deal because you can get your knee artificially replaced when it wears out?
Does your surgeon believe in regenerative medicine? If so he will try to save all the tissue, knowing that more natural tissue is better than less and that joint replacements aren’t the panacea they are hyped to be? Or does your surgeon believe in meniscus replacement and knows how much to save in order to be able to replace the missing tissue successfully?
Each of these biases affects the approach to your knee. Ask about your surgeon’s outcomes, too. Find out if they truly know their data by outcome studies or if they are using some other way to track how their patients do after surgery. Make sure they’re not just guessing.
Finally, your biases play as big a role, too.
Are you willing to have a longer rehab period in order to permit tissue healing? Are you OK if an effort to save your meniscus fails and you need a follow-up procedure? Do you just want to get back to work quickly and aren’t concerned with the long-term outcomes? Do you want to run marathons and need every bit of shock absorption possible? Have you and your surgeon agreed on the goals of the surgery?
I believe there is tremendous art to surgery and science to the artistry. I believe that every patient and every problem is unique and that it’s important to try to match the surgeon’s skills with the patient’s needs. Part of a surgeon’s job is to educate patients not just about what we can do today but what the future is bringing in terms of new techniques and understanding.
If you’re told that your procedure is “standard,” remember to ask, “Who is standard?” Standard procedure certainly does not fit in my vocabulary.