New technology being introduced at NYU Langone Medical Center could help researchers advance blood biomarker capabilities that show changes in low concentrations of specific proteins present following a neurological injury.
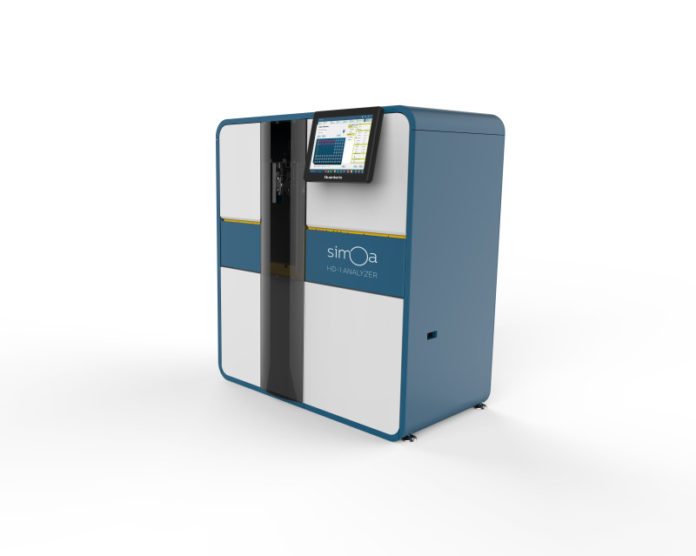
The single molecule array (Simoa) technology developed by Quanterix, and the fully automated HD-1 analyzer, offers unprecedented improvement in protein sensitivity over current technologies for the detection of blood-based biomarkers — as much as 1,000 times more sensitive than conventional immunoassays. Specifically, it allows for more effective measurement of low concentration of proteins, such as tau — a normal protein that is released from brain cells following a brain injury. Utilizing this technology, researchers hope to develop and validate a simple, more objective blood biomarker for the diagnosis, prognosis and treatment of traumatic brain injury (TBI).
“This diagnostic advancement provides us with a more precise ruler for measuring the effectiveness of diagnosis, treatment and progression of TBI,” says Mony J. de Leon, EdD, director of the Center for Brain Health at NYU Langone, professor of psychiatry and an investigator with NYU’s Steven and Alexandra Cohen Veterans Center. “We know that increased tau proteins in the cerebrospinal fluid are a marker for TBI. Having more immediate and consistent access to tau measurements from the blood or saliva will allow us to more accurately determine if a brain injury has, indeed, occurred, and how well a patient is responding to treatment.”
Until recently, there have been limits in tissue availability and technology to detect specific proteins and other potential biomarkers in the blood following TBI. Analyzing cerebrospinal fluid (CSF) has been the most common approach to date to measure these proteins. However, this requires an invasive procedure, and it is not always available or obtainable with certain injuries. Nor is it regularly used to monitor progression and recovery because of its invasive nature.
The result is that a large number of people whose brains appear normal on standard tests (X-ray, computed tomography, or magnetic resonance imaging) could actually have some form of injury whose course is not well understood. “This presents a unique opportunity to develop a mechanisms-based classification of TBI in the context of personalized medicine,” adds Andreas Jeromin, PhD, scientific and medical advisor to Quanterix, Inc.
With further studies, researchers also feel that the technology has the potential to move beyond the clinical spectrum and into military battlefields, sports arenas and other settings where TBI, concussions and other head injuries often occur. In fact, the Simoa technology was recently selected as a winner of the 2014 GE and NFL Head Health Challenge from more than 400 entries across 27 countries by a panel of leading healthcare experts in brain research.
An estimated 1.7 million Americans suffer a traumatic brain injury each year, according to the Centers for Disease Control and Prevention, and an estimated 5.3 million individuals — approximately two percent of the U.S. population — are living with disability as a result of TBI. Traumatic brain injuries can occur from even the slightest bump or blow to the head.
“The Quanterix Simoa will accelerate the discovery of new biomarkers to identify TBI and the development of new treatments, including targeted medications and other therapies,” says Charles L. Marmar, MD, the Lucius Littauer professor and chairman of Psychiatry at NYU Langone and executive director of the Cohen Veterans Center. “It is truly a breakthrough for advancing detection and treatment of brain injuries.”
The addition of the Simoa technology will continue to strengthen the collaborative partnership between TBI researchers at NYU Langone and the Steven & Alexandra Cohen Foundation. In 2014, the foundation made a major $17 million gift to establish the Steven and Alexandra Cohen Veterans Center at NYU Langone. The foundation’s latest gift will fund the purchase of the Simoa technology and support Dr. de Leon’s research to study its use as a potential biomarker for TBI.
“Finding a biomarker to detect PTS and TBI is critical to identifying which veterans need treatment, what kind of treatment, and how we track their progress in getting better,” says Mr. Cohen. “We owe it our veterans to make sure they get the treatment they need and deserve.”
Dr. de Leon also points out that brain injury increases the risk for future neurodegenerative disorders such as Alzheimer’s disease. “Since both TBI and Alzheimer’s share features such as neurofibrillary pathology, and a variant of the tau molecule, the Quanterix device offers opportunities to further explore tauopathy that contributes to Alzheimer’s disease risk,” Dr. de Leon adds.
“We are delighted that NYU Langone and the Cohen Foundation have recognized the value of our Simoa technology for this important project and look forward to how their findings can revolutionize healthcare and precision medicine in the field of TBI,” said Kevin Hrusovsky, executive chairman at Quanterix.
Story Source:
The above story is based on materials provided by NYU Langone Medical Center. Note: Materials may be edited for content and length.