Can a bacterial virus found in Jerusalem sewage prevent infections after root canal procedures?
Every year, drug-resistant infections kill more than 50,000 people across Europe and the United States, and hundreds of thousands more around the world. According to the Review on Antimicrobial Resistance commissioned by the UK Prime Minister, failing to address the growing problem of drug-resistant infections could cause 10 million deaths a year and cost up to $100 trillion USD by 2050.
Now, researchers from the Hebrew University of Jerusalem’s Faculty of Dental Medicine propose a way to turn the tables on harmful bacteria that infect humans, by infecting them with tiny viruses called bacteriophages. In a strange twist, one such virus, cultivated from Jerusalem sewage, may help prevent infections following dental procedures.
Just a few decades ago, antibiotics were considered wonder drugs. Ironically, because they worked so well, they were used too often, leading to the rise of drug-resistant bacteria. These untreatable pathogens evolved mutations enabling them to resist the antibiotics that doctors prescribe to fight them.
One such pathogen is Enterococcus faecalis, a bacterium inhabiting the gastrointestinal tracts of humans. This life-threatening pathogen causes diseases ranging from endocarditis (a potentially fatal heart infection) to bacteremia (harmful bacteria in the bloodstream), as well urinary tract infection, meningitis, and post-treatment root canal infections.
E. faecalis is a highly durable strain, and is especially hard to target when grouped in a sticky bacterial cluster called biofilm. E. faecalis is often recovered from persistent infections associated with root canal treatments, and infection may persist in 20-33% of root canals.
The frustrating rate of infections reflects the limitations of current treatment options. Thus it is essential to develop additional ways to target highly virulent bacteria such as E. faecalis, especially when in biofilm form.
A promising alternative approach to traditional antibiotics is bacteriophage therapy. Bacteriophages, or “phages,” are viruses that infect bacteria. Phages play a key role in maintaining the natural balance in their predator-prey relationship with bacteria. They co-evolved with their bacterial hosts to be highly effective specific “professional bacterial killers.”
Now, a research team — led by Dr. Ronen Hazan from the Institute of Dental Sciences at the Hebrew University, and Dr. Nurit Beyth from the Hebrew University-Hadassah School Of Dental Medicine, together with their co-workers and students, Dr. Shunit Glaser, Leron Khalifa, Daniel Gelman and Yair Brosh — has identified a way to use phage therapy to target E. faecalis biofilms.
The researchers isolated an anti-E. faecalis phage from sewage effluents retrieved from a Jerusalem sewage treatment facility. The phage, named EFDG1, is capable of infecting the V583 strain of E. faecalis, which is resistant to vancomycin, the most effective anti-E. faecalis antibiotic.
The team evaluated EFDG1’s efficacy against E. faecalis cells both in a liquid culture and in biofilm form. Since there are currently no effective ways to eradicate E. faecalis biofilms, the researchers’ goal was to target E. faecalis in its most robust form, as a biofilm.
In both cases EFDG1 almost entirely eradicated the bacterial cultures. EFDG1 was found to be highly efficient against various E. faecalis and E. faecium isolates, regardless of their antibiotic resistance profile.
Moreover, the researchers showed that EFDG1 was highly effective in root canal infection, both in vitro and ex vivo in tissue samples. These findings suggest that phage therapy using EFDG1 might be an effective way to prevent E. faecalis infection following root canal procedures.
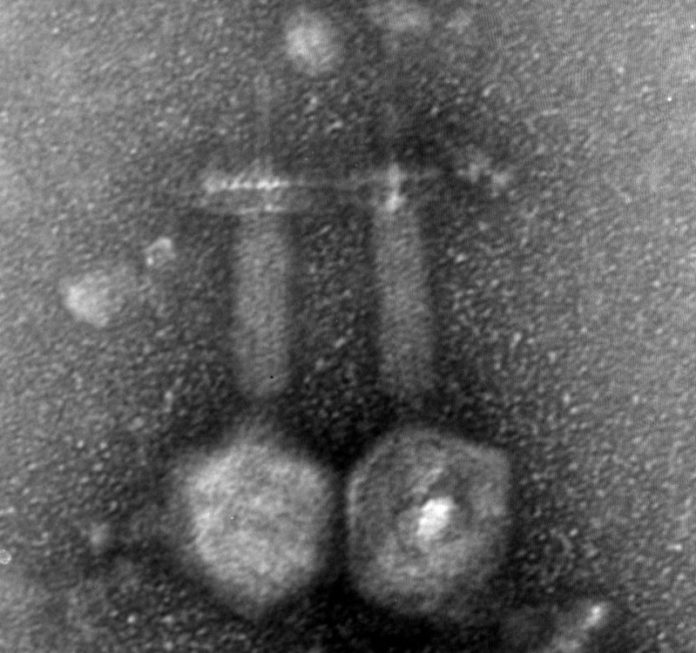
To see whether the EFDG1 is safe to use in fighting E. faecalis infections in humans, the researchers examined EFDG1 phages for the presence of hazardous genes. By visualizing the phage using electron microscopy, followed by whole genome sequencing, the researchers found that it belongs to the Spounavirinae subfamily of the Myoviridae phages, which include other promising candidates for therapy against Gram positive pathogens. Moreover, they found that the EFDG1 genome does not contain apparent harmful genes.
According to Dr. Ronen Hazan, “The idea of using phages as anti-bacterial drugs is not new. Phage therapy was first proposed at the start of the 20th century, but then abandoned for various reasons, including the striking success of chemical antibiotics. Now we stand on the verge of a new era with the limitations of synthetic antibiotics and the emergence of antibiotic-resistant strains of bacteria. Thus it is the right time to look again into what Mother Nature offers in the battle against bacteria. As this research shows, bacteriophages may prove an effective tool in the development of much-needed new antimicrobial drugs.”
The research will appear in the April 2015 edition of the journal Applied and Environmental Microbiology as “Targeting Enterococcus faecalis biofilm using phage therapy.”
The research was supported by a Hebrew University / Yissum startup grant.
Story Source:
The above story is based on materials provided by Hebrew University of Jerusalem. Note: Materials may be edited for content and length.
Journal Reference:
- Leron Khalifa, Yair Brosh, Daniel Gelman, Shunit Coppenhagen-Glazer, Shaul Beyth, Ronit Poraduso-Cohen, Yok-Ai Que, Nurit Beyth, Ronen Hazan. TargetingEnterococcus faecalisbiofilm using phage therapy. Applied and Environmental Microbiology, 2015; AEM.00096-15 DOI: 10.1128/AEM.00096-15