Indigenous Australians in the Northern Territory who require surgery die an average of 12 years younger than the general population, an audit has found, because they suffer from higher rates of illnesses which make surgical procedures riskier or impossible to perform.
A report on the Audit of Surgical Mortality, published in the ANZ Journal of Surgery on Friday, examined 190 deaths between June 2010 and June 2013, of which 72 were of Indigenous Australians.
It found Indigenous Australians admitted to hospital in the Northern Territory with surgical conditions died at an average age of 53, compared to 65 for non-Aboriginal Australians.
Most of those deaths occurred during general surgery, the audit found. Although quality of care was equal among all patients, Indigenous people suffered a significantly higher rate of additional diseases, known as comorbidities, at their time of death, including diabetes, liver disease and kidney disease.
Almost one quarter of Aboriginal patients had an infection at their time of death.
A lead author of the report, Royal Australasian College of Surgeons chair Dr Peter Treacy, said the results were “no surprise”, as it was well known Aboriginals suffered a higher burden of disease.
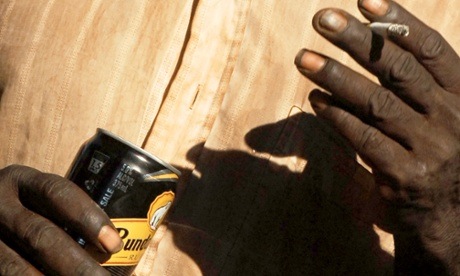
“We strongly suspect alcohol abuse, smoking and diabetes are leading to a lot of these comorbidities,” Treacy, a general surgeon in Darwin, said.
“The failure is knowing where and how to address these issues. This audit has highlighted exactly which conditions are prevalent, and at least directs us to where we can focus disease prevention and control efforts.”
Treacy said he was optimistic improvements were already occurring as a result of better housing and sanitation in some areas of the Northern Territory.
A co-author of the report, Dr John North, said it was important that elders within Indigenous communities led public health education efforts.
“This report suggests the alcohol situation in these communities is out of control,” he said.
“Really the leaders and elders of the Aboriginal community need to take control of that, because politicians have tried and they can’t do it.
“Decisions and interventions have to be led by the people themselves. I’ve been heavily involved with Aboriginal communities in Queensland, and it’s just so terrible to see alcohol and other drugs causing unbelievable destruction for the first Australians.”
In an editorial accompanying the report, Truskett described the audit results as “alarming”.
“As a professional body, we cannot ignore this alarming discrepancy in life expectancy in our Indigenous population, and we need to play a constructive advocacy role,” he wrote.
The audit results follows the release of the Closing the Gap report on Wednesday, which found Australia was failing to close the gap in the disadvantage of Indigenous people, with little to no progress being made in improving life expectancy.
While Indigenous health outcome targets were achievable, not enough effort was being made to meet them, the report also found.
But Dr Mahiban Thomas, a maxillofacial and oral surgeon at Royal Darwin hospital, is trying to improve the situation. He is trialling some innovative programs to improve the healthcare and life expectancy of Indigenous Australians.
“With Indigenous health, unfortunately, you can’t put together a pretty two-sentence statement about how to address key issues,” Thomas said.
“One area we are focusing on within my work is to try to take healthcare to Indigenous people where they are living, so they don’t have to travel.
“For elective surgery, we are trying to move Aboriginal patients requiring surgery to clinics as a group, because they are more willing to travel as a group as a sense of community is important to them, and there are tribal instincts at play.”
He hoped these programs would see the healthcare gap close within a generation.
“We are trying to do what we can, but we don’t want to say it is working until we have done it for long enough to gather the evidence,” he said.
“It can take a generation for positive changes to be seen”