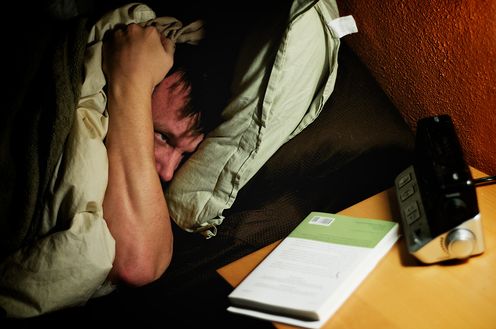
We all have a poor night’s sleep from time to time: those nights when you lie awake for hours trying desperately to go to sleep but can’t stop worrying about tomorrow. Or when you repeatedly wake up throughout the night, or can’t get back to sleep in the early hours of the morning.
One-third of the world’s population experience short-term sleeping difficulties. These usually last only a few weeks. But for an unlucky 3% of Australians, these sleep disturbances may last a lot longer and lead to a diagnosis of insomnia.
A person with insomnia is unable to fall asleep, stay sleep, and/or wakes up too early at least three times a week for at least three months. This can lead to considerable distress.
Sufferers experience persistent tiredness, low energy and difficulties with concentration, attention and memory. They may feel down, stressed or anxious, not only about getting a good night’s sleep but about their ability to do their daily activities.
What causes insomnia?
Biological, social and psychological factors interact to trigger and maintain sleeping difficulties.
Biological factors include changes to the body’s natural 24-hour body clock, or circadian rhythms, which control the timing of when we feel sleepy and awake throughout the day. Circadian rhythms are sensitive to body temperature, light and physical alertness. When there is too much or too little of a combination of these factors, the body doesn’t release enough sleep-inducing hormones such as melatonin to feel sleepy.
Social factors, such as shift work or frequent international travel, can contribute by causing our body clock to become out of sync with the environment it’s in. Our bodies adjust slowly to these changes and depend on our being able to get sunlight exposure and exercise.
Psychological factors, including unhelpful thoughts (“I’m never going to get to sleep tonight”) and behaviours (watching the clock during the night), can reduce the amount and quality of sleep a person gets.
These factors interact in complex ways. Sleep sensitivity, or a family history of sleep disturbance, for example, make some individuals vulnerable to developing insomnia because they’re more likely to have their sleep disturbed by stressful events, such as a relationship breakdown.
Being unable to fall asleep often leads to bedtime worrying, which makes it even harder to fall asleep. To try to make up for a lack of sleep, you might then start going to bed earlier, sleep in or take daytime naps. Over time, these unhelpful thoughts and behaviours can create a cycle that makes the insomnia worse.
How do you treat insomnia?
Successful treatment of insomnia requires getting help to change as many of the interacting factors as possible, rather than trying one or two things in isolation. This is what cognitive-behavioural therapy, or CBT, tries to do.
CBT re-trains people to view the bedroom as a place of sleeping instead of a place where they lie awake tossing and turning and worrying about not sleeping. CBT also helps people change their lifestyle and sleeping environment, learn relaxation skills and challenge the unhelpful worries and beliefs that contribute to insomnia.
CBT has been found to reduce sleeping difficulties by 50% on average, and reduces insomnia symptoms to a level where they are no longer considered clinically severe.
When people visit their GP for insomnia treatment, they’re often encouraged to use many of the techniques CBT uses. But these skills are difficult to teach in a short consultation, so many patients don’t use them.
Sleeping medications may then be prescribed to help a person fall asleep and stay asleep when correctly used for a short period. But sleeping medications only provide short-term relief and can be harmful or addictive if used longer term.
If your symptoms persist, your GP may refer you to a specialist doctor or psychologist for CBT.
Another credible alternative is web-based treatment. Research from Japan to America shows that, for some people, online insomnia treatment modules may be as effective as visiting a health professional in person.
We’re piloting a seven-week, interactive CBT program to help Australians with insomnia, called Sleep-e. So far, the data looks promising, suggesting it can reduce the severity of insomnia in people waiting for treatment at a public hospital-based insomnia clinic.
To get a good night’s sleep, try to establish a relaxing bedtime routine. Limit the use of computer tablets and mobile devices before bed. If you can’t sleep, get up and do a relaxing activity, such as reading a book, and return to bed only when you feel sleepy again.
Online programs can help you to practise good sleep hygiene habits, change unhelpful sleeping patterns and reduce the worry that can contribute to insomnia, helping you to get a better night’s sleep.
For further information about Sleep-e see Mental Health Online or email the research team. Other online programs are available for a fee, including SHUTi and Sleepio.
Hailey Meaklim receives funding from The Barbara Dicker Brain Sciences Foundation. She is affiliated with the Australasian Sleep Association.
Jo Abbott receives funding from The Barbara Dicker Brain Sciences Foundation.
Imogen Rehm does not work for, consult to, own shares in or receive funding from any company or organisation that would benefit from this article, and has no relevant affiliations.