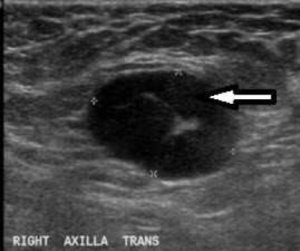
Which breast cancer patients need to have underarm lymph nodes removed? Mayo Clinic-led research is narrowing it down. A new study finds that not all women with lymph node-positive breast cancer treated with chemotherapy before surgery need to have all of their underarm nodes taken out. Ultrasound is a useful tool for judging before breast cancer surgery whether chemotherapy eliminated cancer from the underarm lymph nodes, the researchers found. The findings are published in the Journal of Clinical Oncology.
In the past, when breast cancer was discovered to have spread to the lymph nodes under the arm, surgeons routinely removed all of them. Taking out all of those lymph nodes may cause arm swelling called lymphedema and limit the arm’s range of motion.
Now, many breast cancer patients receive chemotherapy before surgery. Thanks to improvements in chemotherapy drugs and use of targeted therapy, surgeons are seeing more women whose cancer is eradicated from the lymph nodes by the time they reach the operating room, says lead author Judy C. Boughey, M.D. a breast surgeon at Mayo Clinic in Rochester.
The current study finds that repeating ultrasound after chemotherapy is a sound way to help determine whether surgeons should remove only a few lymph nodes and test them for cancer, sparing patients whose sentinel nodes are cancer-free the removal of all nodes in the armpit, or take out all of the nodes, Dr. Boughey says.
“Our goal here is really to try to get away from, ‘Every patient with breast cancer needs these drugs, and this amount of chemotherapy and this surgery,’ and instead to personalize surgical treatment based on how the patient responds to chemotherapy,” Dr. Boughey says.
Avoiding complete underarm lymph node removal when possible means fewer women will experience the complications that can accompany that surgery, and avoiding those side effects should also save health care costs, she says.
“That’s one of the really nice things about giving chemotherapy up front: It allows us to be less invasive with surgery, both in terms of breast surgery and lymph node surgery, and to tailor treatment based on response to chemotherapy,” Dr. Boughey says. Most patients with lymph node-positive breast cancer receive radiation treatment after surgery. A new study is under way for men and women with breast cancer whose underarm lymph nodes are still positive for cancer after chemotherapy. It will evaluate which is more effective: removing all of those nodes, or leaving the nodes and treating them with radiation, Dr. Boughey says.
Story Source:
The above story is based on materials provided by Mayo Clinic. The original article was written by Sharon Theimer. Note: Materials may be edited for content and length.
Journal Reference:
- J. C. Boughey, K. V. Ballman, K. K. Hunt, L. M. McCall, E. A. Mittendorf, G. M. Ahrendt, L. G. Wilke, H. T. Le-Petross. Axillary Ultrasound After Neoadjuvant Chemotherapy and Its Impact on Sentinel Lymph Node Surgery: Results From the American College of Surgeons Oncology Group Z1071 Trial (Alliance). Journal of Clinical Oncology, 2015; DOI: 10.1200/JCO.2014.57.8401