Tens of millions of people around the world have abnormal, leak-prone sproutings of blood vessels in the brain called cerebral cavernous malformations (CCMs). These abnormal growths can lead to seizures, strokes, hemorrhages, and other serious conditions, yet their precise molecular cause has never been determined. Now, cardiovascular scientists at the Perelman School of Medicine at the University of Pennsylvania have studied this pathway in heart development to discover an important set of molecular signals, triggered by CCM-linked gene defects, that potentially could be targeted to treat the disorder.
“We hope that these findings will lead to a better understanding of the origins of CCM, and thus to treatment possibilities,” says Mark L. Kahn, MD, a professor of Cardiovascular Medicine, and senior author of the new study, published in Developmental Cell.
Although CCM has a relatively high prevalence of 1 in 200 people worldwide, it typically goes undiagnosed until symptoms arise and can only be treated by brain surgery.
Research on CCM has been slowed by the difficulty of recreating the disease in lab animals. About 20 percent of CCM patients have a highly aggressive, inherited form of the disorder that is caused by inactivating one of three genes, whose protein products normally work together in a complex. But knockout mice bred without a full set of those genes don’t mature to have CCMs in their brains–they die in the womb, having failed to develop a working vascular system.
“Those animals die so early in their development that you just don’t get enough information about what the genes normally should be doing,” Kahn says.
Studies by Kahn’s lab and others have shown that CCM gene knockouts remain lethal to fetal mice even when they are limited to the endothelial cells that line blood vessels and the heart.
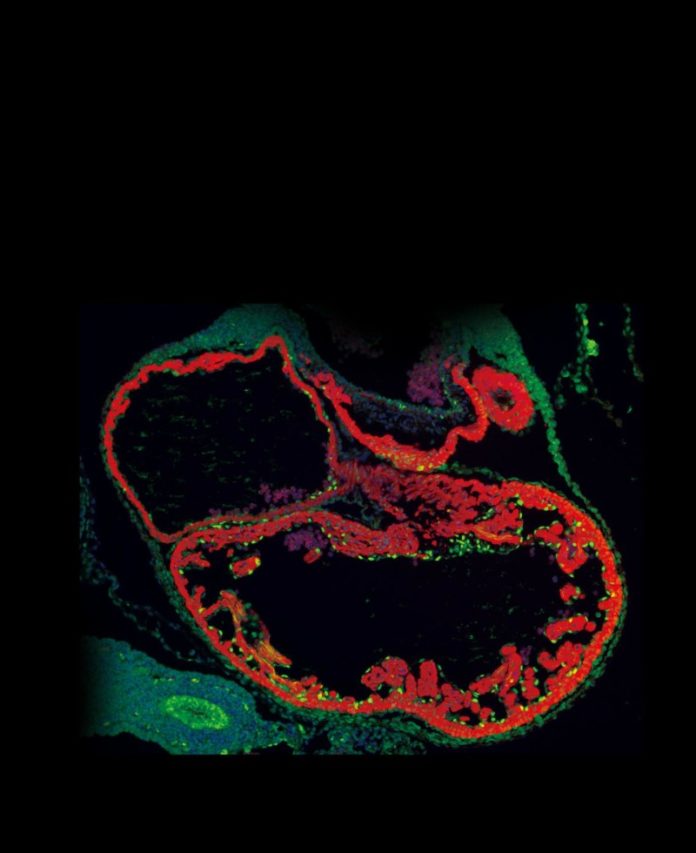
In the new study, Kahn and colleagues used advanced techniques to restrict CCM gene disruption to the endothelial cells of the developing heart, leaving the mouse vascular system to develop otherwise normally.
The resulting mice still died before birth, this time from a failure of normal heart development, which is not seen in human CCM patients. But they survived in the womb about a week longer than standard CCM knockout mice. That allowed Kahn’s team to learn more about the effects of the gene disruptions, and ultimately to find a previously unknown CCM-related signaling pathway.
An initial clue was that the mice developed an abnormally thin layer of heart muscle. A substance known as “cardiac jelly” that should separate the developing heart muscle from the heart endothelium in healthy mice was severely reduced. Analyses of gene expression changes revealed that the CCM-disrupted heart endothelial cells were overproducing protease enzymes that degrade cardiac jelly. Suppressing the activity of the protease genes largely prevented the heart defects.
Kahn’s team traced the triggers of the protease gene overactivity back to a signaling protein called MEKK3, which helps drive cell growth and survival and has been implicated in cancers. Reducing MEKK3 activity shut down the jelly-degrading protease genes and mostly prevented the heart defects. Experiments also showed that MEKK3 bound to the CCM-complex proteins, whose absence causes familial CCM disease.
More than a decade ago, other researchers noted that MEKK3 somehow associated with one of the CCM-complex proteins. “That observation didn’t really lead anywhere because at the time our understanding of the CCM pathway was minimal,” says Kahn. Now it appears that, at least in the endothelial cells of the developing heart, CCM proteins normally bind MEKK3, and when they are absent, MEKK3 becomes abnormally–and harmfully–active.
A key question now is whether overactive MEKK3 also contributes to the brain vascular malformations of CCM disease. The Kahn lab is addressing that question by studying MEKK3 activity in a recently developed CCM mouse model. In this animal model, the deletion of CCM genes in endothelial cells shortly after birth produces vascular lesions in the brain that closely resemble those of human CCMs.
“If we can show that MEKK3 signaling leads to CCMs in that model, then it will be time to think about what the best therapeutic strategy will be,” he said.
Story Source:
The above story is based on materials provided by University of Pennsylvania School of Medicine. Note: Materials may be edited for content and length.