Once thought to be a problem only in poorly regulated jurisdictions overseas, unproven stem cell treatments are increasingly being offered in Australia. Now, the Therapeutic Goods Administration (TGA) is holding a public consultation on whether current regulation of treatments that involve using the patient’s own cells is appropriate.
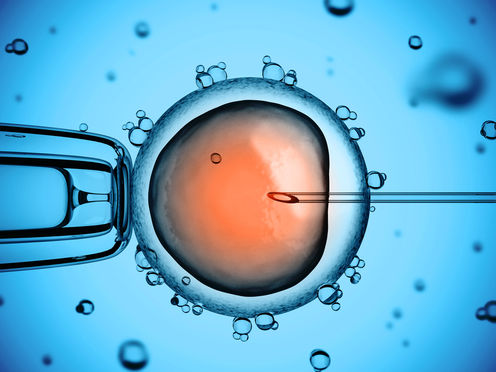
Stem cell science has captured the public’s imagination. The possibility that we can replace or repair damaged cells seems an obvious and relatively straightforward procedure. In some cases it is. People with leukaemia and other diseases of the blood system, for instance, have benefited from blood stem cell transplants for many decades.
But that doesn’t mean we can simply give diabetic patients new insulin-producing cells, or replace the dopaminergic neurons that no longer work in those suffering from Parkinson’s disease. For most medical conditions, there’s much more to learn before stem cell therapy delivers on its promise.
Hope and exploitation
Although researchers have made enormous advances in understanding how to turn stem cells into nerve, heart and other cells of the body over the last decade, translating these discoveries into clinically relevant and approved treatments still needs extensive work. Initially, this is done in the laboratory. Then there’s rigorous testing in properly conducted clinical trials. All this takes time – a lot of it.
The first issue that needs to be addressed is whether the proposed therapy is safe. Given that stem cells have an inherent regenerative capacity, we need to ensure transplanted cells don’t cause harm. Determining this requires careful, long-term monitoring – even when the cells being used are taken from the same person.
Consider the case of a US woman who had (failed) stem cell therapy for paraplegia. She developed a mucus-secreting growth in her spine eight years after participating in a clinical trial where stem cells from her nose were implanted into her spine.
While fortunately rare, such reports of adverse outcomes highlight how much we still don’t know about these remarkable cells. They also illustrate the need for ongoing due diligence to assess the true possibilities of this new frontier of medical care.
For those suffering from incurable conditions, the time taken to develop stem cell-based therapies is understandably extremely frustrating. And many are not prepared to wait. These are the people who seek out “stem cell” clinics prepared to treat them now – often for a hefty fee.
Most such treatment is done abroad and is known as stem cell tourism. Indeed, it was initially thought to be limited to countries such as India, China, Mexico and the Bahamas – all jurisdictions with limited regulatory regimes that have little recourse to intervene in the sale of unproven treatments.

But over the last couple of years, Australian clinics selling stem cell treatments have begun offering what people seeking unproven treatment used to have to travel abroad to access. Because the treatments are being offered locally, they have an implied legitimacy despite the lack of reputable evidence in their support.
A regulatory loophole
The TGA already imposes stringent standards on the manufacturing of cells for therapy, but these regulations are currently limited to donated cells. The use of the patient’s own cells (no matter how they are produced and given back to the patient) remains broadly unregulated.
This means that rather than having to collect evidence in a registered trial before they take their product to the clinic, some Australian doctors are selling what is effectively experimental therapy.
The going rate of around A$10,000 may not seem much to charge for a much-hoped-for improvement. But, in most cases, there’s not only an absence of evidence for benefit, the risks of the therapy are also unknown.
Typically, crude cell preparations taken from fat and from blood are being injected into joints, and also back into veins, for conditions ranging from multiple sclerosis and Parkinson’s disease to arthritis. And treatment is often part of a fly-in-fly-out procedure by doctors who may not be recognised experts in the disease.
The possibility of infection, inappropriate cell growth or much more serious complications, such as pulmonary embolism – where the cells are trapped in the lung and block blood supply – are very real.
What’s more, there’s often no provision for long-term follow-up, which means potential adverse effects can be overlooked. The long-term impact of the treatment on the course of the disease is never documented.
Stem cell science is a new and exciting area of medicine, but enthusiasm and hope need to be tempered with reliable evidence. Providing unproven treatments outside the normal regulatory and clinical trial framework has the potential to undermine public confidence in this field and obstruct the development of new therapies with real benefits.
As outlined in the TGA discussion paper launched with the announcement of the consultation, several straightforward modifications to current Australian regulations could curb the worst of these practices. And avoid putting patients and, indeed the sector, at an unacceptable risk.
Megan Munsie receives funding from the Australian Research Council. She is affiliated with International Society for Stem Cell Research and the Australasian Society for Stem Cell Research.
Martin Pera receives funding from the ARC, NHMRC, and the Human Science Frontiers Program.