Race has a powerful influence on whether women diagnosed with breast cancer will survive the disease, a new study reveals. The findings, published in the Journal of the American Medical Association, indicate that black women are more likely than women of other races to die from the disease, even when their tumors are diagnosed at an earlier stage when they are small and theoretically easier to treat.
The American Cancer Society estimates that nearly 232,000 women in the U.S. will be diagnosed with invasive breast cancer this year, and more than 40,000 will die from the disease. It has long been known that breast cancer incidence among U.S. women varies by race and ethnicity. Overall, white women are more likely to develop breast cancer than African American women, but African American women are more likely to die from the disease. Among women under the age of 45, however, African Americans are more likely to develop breast cancer, while Asians, Hispanics and native American women are less likely to both develop and die from the condition.
While the causes of breast cancer disparities are complex and numerous, past research has identified several key culprits — namely, lack of health insurance and other social- and health care-related inequities — that contribute to higher mortality rates among African American women.
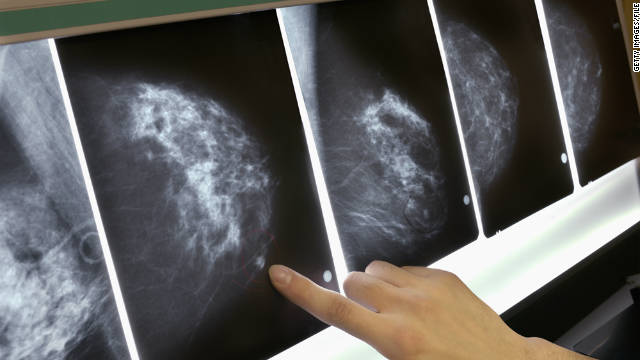
In this latest study, Dr. Steven Narod and his team at Women’s College Hospital in Toronto set out to identify the variation in early-stage breast cancer diagnosis (stage I) by race and ethnicity and determine whether biological differences in tumor aggressiveness play a role in these variations. The authors hypothesized that “the growth rate and metastatic potential of small-sized breast cancer tumors may vary between women due to inherent differences in grade, receptor status and other or unknown pathological features.”
To reach their conclusions, Dr. Narod’s team analyzed the medical records of 452,000 women in the U.S. who were diagnosed with invasive breast cancer between 2004 and 2011. After excluding women with stage 0 or unknown breast cancer, the team were left with 373,563 women in their analysis, who they followed for an average of 40.6 months.
The researchers assessed the biological aggressiveness of small-sized tumors (2 cm or less) across all eight races and ethnicities identified: non-Hispanic white, Hispanic white, black, Chinese, Japanese, South Asian (Asian Indian, Asian Indian or Pakistani, Pakistani), other Asian (Filipino, Thai, Vietnamese, Korean, Kampuchean, Laotian, Hmong) and other ethnicities (including Native American and Alaska Native). By race/ethnic group, the team also assessed the women’s risk of being diagnosed with breast cancer in the early stages of the disease, their likelihood of being diagnosed at a later stage and their risk of death from the disease.
Black women more likely to be diagnosed late, less likely to survive
The analysis revealed that black women were less likely than women of other races to be diagnosed with breast cancer when the tumor was in an early stage, and that they were more likely to have small tumors that spread throughout the body. While 50.8 percent of non-Hispanic white women were diagnosed with breast cancer at stage I (the earliest stage), only 40.4 percent of South Asian women and 37 percent of black women were diagnosed at that early stage.
The results also showed that black women had a higher risk of death seven years after being diagnosed with stage one breast cancer, compared to non-Hispanic white women and other racial and ethnic groups, including women from South Asia, with 6.2 percent, 3 percent and 1.7 percent dying from the condition, respectively. In addition, the researchers found that black women were much more likely to die from small-sized breast cancer tumors than non-Hispanic white women, at 9 percent compared with 4.6 percent.
The researchers say the differences in diagnosis and survival of stage I breast cancer among racial/ethnic groups may be partially explained by variations in biological variations in tumors, including lymph node metastasis, distant metastasis and triple-negative behavior (in which cancer growth is not driven by estrogen receptors, progesterone receptors and human epidermal growth factor receptor 2 (HER2). “In support of this hypothesis, a black woman with small-sized breast cancer tumors was more likely to present with lymph node metastases, was more likely to have triple-negative cancer and was more likely to present with distant metastases than a non-Hispanic white woman with tumors of similar size,” the authors explain.
Socioeconomic factors may be driving racial disparities in breast cancer mortality
The researchers note that socioeconomic status, access to and use of health care, adherence to treatment and presence of additional health conditions likely also contributed to variations in diagnosis and survival of early-stage breast cancer, but say the findings demonstrate that biological causes are at play. However, Dr. Otis Brawley, chief medical officer of the American Cancer Society, told the Canadian Press that the differences in breast cancer mortality may not be due to race at all, but rather socioeconomic factors that highly correlated with race.
He explained that girls who are born into poor families typically eat unhealthier diets, are more likely to gain weight in childhood, and are more likely to start menstruating at an early age — a known risk factor for breast cancer. He also said studies of an all-white cohort in Scotland found that women who were economically deprived in childhood had increased breast cancer rates later in life and were more likely to develop breast cancer at a younger age than women who were more economically advantaged.
According to Dr. Brawley, the American Cancer Society would expect to see similar survival outcomes among poor white women as among poor black women — and even middle- and upper-income black women who grew up poor. However, as the new study shows, this is not the case. “I believe it’s race for social reasons, and not race for biologic reasons,” Dr. Brawley said. “There are a lot of lifestyle factors that actually do affect biology and change biology.”