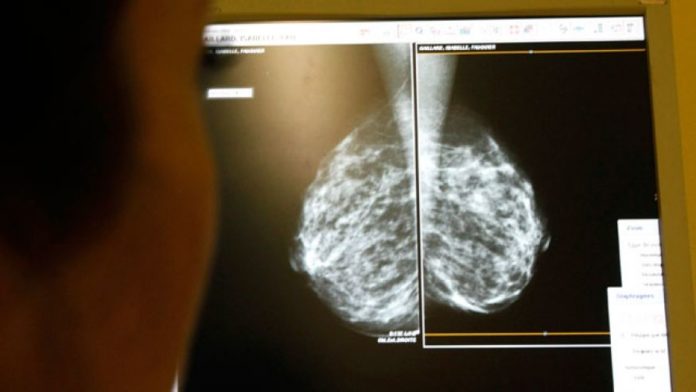
Women with atypical hyperplasia of the breast have long been known to have a heightened risk of breast cancer, but a new Mayo Clinic study finds that the risk may be far higher than previously thought. Results of the study appear in a special report on breast cancer in the New England Journal of Medicine.
Atypical hyperplasia of the breast, also called atypia, is a precancerous condition found in about one-tenth of the more than 1 million breast biopsies with benign findings performed annually in the United States. It is unclear what causes atypia, but it is known that the condition occurs when breast cells become abnormal in terms of size, shape, number, appearance and growth pattern.
Atypia lesions are considered benign, but by its risk and appearance and genetic changes, they exhibit some of the early features of cancer. Moreover, past studies have found that women with atypical hyperplasia have four to five times the relative risk of developing breast cancer — in other words, they are thought to be four to five times more likely to develop breast cancer than those with normal breast cells.
However, the researchers behind this latest study note that there is limited research on the absolute risk of a woman with atypical hyperplasia developing breast cancer — that is, their likelihood of developing the disease over a specific time period. With limited risk data, women with atypical hyperplasia may be missing out on important preventive measures like enhanced screening for breast cancer, the Mayo Clinic team says. A more clearly defined risk could help women and their doctors develop better risk-reduction strategies, they note.
“By providing better risk prediction for this group, we can tailor a woman’s clinical care to her individual level of risk,” says Dr. Lynn Hartmann, M.D., an oncologist at Mayo Clinic and lead author of the study. “We need to do more for this population of women who are at higher risk, such as providing the option of MRI (magnetic resonance imaging) screenings in addition to mammograms and encouraging consideration of anti-estrogen therapies that could reduce their risk of developing cancer.”
Risk of breast cancer increased by 1 percent each year
With this in mind, Dr. Hartmann’s team followed 698 women who had been diagnosed with atypical hyperplasia after undergoing breast biopsies at the Mayo Clinic between 1967 and 2001. The researchers assessed the women’s medical records and monitored their atypia pathology. In addition, all women completed follow-up health questionnaires, from which the researchers were able to gather information on any breast cancer diagnoses.
Over an average follow-up period of 12.5 years, 143 women had developed breast cancer, the researchers found.
On analyzing the women’s absolute risk of breast cancer from the time of biopsy, they discovered that it increased by more than 1 percent each year; 7 percent of women had developed the disease after 5 years, 13 percent had developed it after 10 years, while 30 percent developed breast cancer 25 years after biopsy.
Importantly, these findings were validated by researchers at Vanderbilt University using biopsies from a separate cohort of women with atypia. Both data sets revealed that at 25 years following biopsy, 25 to 30 percent of these women had developed breast cancer.
More accurate risk stratification
After obtaining these initial findings, the team applied information from patients’ pathology specimens to the absolute risk calculations, with the aim of reaching more accurate risk estimates.
While most studies have relied only on statistical models for these calculations, the Mayo Clinic team had previously found that the two most common statistical risk prediction models (the BCRAT and the IBIS models) performed poorly in women with atypical hyperplasia, underscoring the need to provide alternative approaches for predicting risk in this population.

To obtain more accurate risk estimates, the researchers incorporated data from participants’ breast biopsies.
“These models are based on epidemiologic risk factors, such as family history. Such risks have driven the development of atypical hyperplasia and don’t serve to further stratify risk when the phenotype of atypia is present. I would not suggest using these models in this population,” she told the American Society for Clinical Oncology’s ASCO Post.
When they incorporated the pathology data, the team found that a woman’s risk of breast cancer increased along with the intensity of atypia in a patient’s biopsy, determined by the amount of separate clusters of abnormal breast cells.
In the case of women with three or more clusters of abnormal breast cells in their biopsies, for example, 47 percent had developed breast cancer 25 years after biopsy, compared with only 24 percent of women who had one cluster.
“Instead of relying on a statistical model, our study provides actual data of breast cancer cases that occurred in a population of women with atypia. These absolute risk data are preferable to a hypothetical model,” says Amy Degnim, M.D., co-lead author and a breast surgeon at Mayo Clinic.
Women with atypical hyperplasia should be considered high-risk
Based on these results, the researchers recommend that women with atypical hyperplasia be recognized as having significantly increased lifetime risk of breast cancer and thus be candidates for screening MRI.
The American Cancer Society (ACS) has said that an MRI scan is worthwhile for women whose lifetime risk of breast cancer is 20 to 25 percent. Currently, Dr. Hartmann said, women with hyperplasia are not considered to meet that cutoff; these new findings may challenge that.

Based on their findings, the authors say women with atypical hyperplasia should discuss MRI breast screening with their doctors.
“Most of the published guidelines state only relative risk data for atypical hyperplasia or a lower lifetime risk, such as 15 percent, which does not qualify them for screening magnetic resonance imaging. Their high cumulative risk is not yet recognized,” she told ASCO Post.
Moreover, anti-estrogen medications like tamoxifen (which are also referred to as chemoprevention) have already been tested in clinical trials in women with atypical hyperplasia and shown to lower their risk of breast cancer by 50 percent or more. Yet, Dr. Hartmann says, many women with atypical hyperplasiaare not taking the medications, in part because they and their physicians have not had solid estimates of their breast cancer risk to guide them.
“Many women are reluctant to use these drugs because of a fear of side effects, but physicians are also reluctant to prescribe them, especially family physicians, who report being unfamiliar with the agents and their side-effect profiles,” she told ASCO Post. “Chemoprevention in this particular high-risk population should be encouraged.”
Commenting on the team’s findings, Dr. Laura Kruper, a breast surgeon and co-director of the Breast Cancer Program at City of Hope Cancer Center in Duarte, Cali., told US News the takeaway message is that “atypical hyperplasia is much more serious than we have been taking it”.
“When you say a cumulative risk of 30 percent at 25 years, that is pretty serious,” Dr. Kruper said. “We as a medical community need to pay more attention to this.”