Common variations in four genes related to brain inflammation or cells’ response to damage from oxidation may contribute to the problems with memory, learning and other cognitive functions seen in children treated for acute lymphoblastic leukemia (ALL), according to a study led by researchers from Boston Children’s Hospital, The Children’s Hospital at Montefiore, and Dana-Farber/Boston Children’s Cancer and Blood Disorders Center.
The data, presented at the 56th annual meeting of the American Society of Hematology, suggest that it may be possible to genomically screen ALL patients for their risk of long-term treatment-related effects on memory, attention and learning and to study potential interventions.
“Our goal is to be able to identify who is at risk for cognitive late effects and provide neuroprotective interventions,” said study senior author Deborah Waber, PhD, senior associate in psychiatry and director the Learning Disabilities Program in Boston Children’s Department of Neurology, who has spent 30 years studying the relationship between cognitive decline and ALL therapy, including cranial radiation and/or chemotherapy to the central nervous system. “This retrospective analysis tells us that going forward we may wish to examine children’s genotypes at baseline and conduct prospective research to learn why these specific gene variants may increase risk of toxicity.”
ALL is the most common childhood cancer, with survival rates of around 90 percent. ALL patients receive chemotherapy to the central nervous system, and some receive cranial radiation, in order to eliminate cancer cells that can lurk in the brain and raise their risk of relapse. ALL survivors often experience problems with persisting attention, memory and learning, which have been documented by neurocognitive studies conducted in the years after completion of curative treatment.
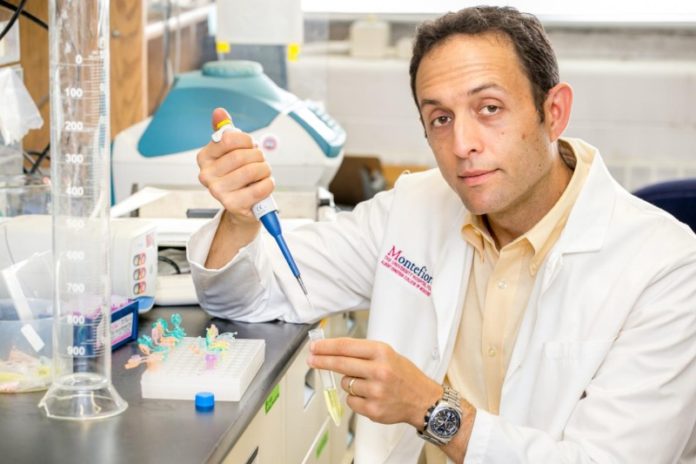
“The more we look, the more we find that many survivors experience changes in how they think,” said study lead author Peter Cole, MD, a pediatric hematologist/oncologist at The Children’s Hospital at Montefiore and associate professor of pediatrics at Albert Einstein College of Medicine of Yeshiva University. The variability in these changes, he added, raises an interesting question: “If we give all ALL patients the same treatment, why is it that some of them experience memory or cognitive deficits, but not all of them?”
To determine whether inherited genetic variations might have roles to play, the research team gathered stored blood samples and cognitive function test data (e.g., IQ, memory, attention span, hyperactivity behaviors) on 350 ALL survivors treated at eight centers in the United States and Canada. All of the survivors had been treated on one of two consecutive Dana-Farber Cancer Institute ALL Consortium therapy protocols, 95-01 (1996-2000) or 00-01 (2000-2004).
The researchers then examined each survivor’s genome for common variants in 28 genes involved in drug metabolism or cellular damage responses, and then compared the results against the cognitive data.
“We limited ourselves to variants that are present in at least 10 percent of the population, deciding that we were interested in explaining what could be happening in most patients,” Cole said.
After controlling for factors such as age at diagnosis, sex, socioeconomic status and whether the child received radiation to the brain, the research team found that variants in four genes–NOS3, SLCO2A1, HFE and COMT–were significantly associated with neurocognitive effects. All four are members of pathways that regulate inflammation in the brain or protect cells from oxidative stress, a form of cellular damage caused by chemotherapy.
The researchers note that the retrospective nature of the study means they cannot prove that the gene variants themselves increased patients’ risk of poor neurocognitive outcomes. They are now conducting prospective studies to try to establish that link. Any potential protective interventions would also need to undergo preclinical and clinical testing to rule out the risk of interactions that could negatively impact a patient’s likelihood of being cured.
“A major ongoing priority in childhood ALL clinical research is to reduce the toxicity of treatment, and certainly we want to reduce neurocognitive late effects if possible,” said Lewis Silverman, MD, clinical director of the Hematologic Malignancy Center at Dana-Farber/Boston Children’s, principal investigator of the DFCI ALL Consortium clinical trials group, and a co-author on the study. “Hopefully this work will lead to a way to identify those patients at highest risk of neurocognitive late effects in whom we can focus our research efforts–adjusting our treatment approach or testing novel protective strategies with the goal of reducing the neurocognitive late effects without adversely impacting the chance for cure.”
Story Source:
The above story is based on materials provided by Dana-Farber Cancer Institute. Note: Materials may be edited for content and length.