Researchers from Brigham and Women’s Hospital (BWH) have identified what they believe to be the cells responsible for fibrosis, the buildup of scar tissue. Fibrotic diseases, such as chronic kidney disease and failure, lung disease, heart failure and cirrhosis of the liver, are estimated to be responsible for up to 45 percent of deaths in the developed world.
The findings are published online in the journal Cell Stem Cell.
“Previous research indicated that myofibroblasts are the cells responsible for fibrosis,” said Benjamin Humphreys, MD, PhD, senior author of the research paper and a physician scientist in the Renal Division at BWH. “But there was controversy around the origin of this cell. Identifying the origin could lead to targeted therapies for these very common diseases.”
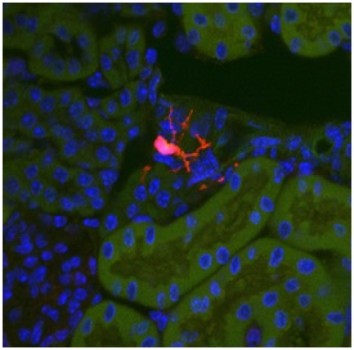
With the knowledge that fibrosis appears to radiate from blood vessels, Humphreys and colleagues examined the hedgehog signaling pathway, which normally regulates organ development but whose roles in the adult are less clear. They noticed that in adult mice, a hedgehog pathway gene called Gli1 was specifically expressed in a rare group of cells located around blood vessels in all solid organs. This pattern suggested that the cells might play a role in fibrosis. To test this hypothesis the researchers tagged this protein in tissue with varying forms of fibrosis, and found that these cells proliferated by almost 20-fold under chronic injury and turned into myofibroblasts.
“We believe that this cell population is responsible for about 60 percent of all organ myofibroblasts,” said Humphreys.
After identifying these cells, first author Rafael Kramann, MD, Humphreys and colleagues set out to determine whether removing these cells would lead to improvement in organ function.
Using a genetic strategy in mice, the researchers were able to ablate these Gli1 cells, while leaving other cells unharmed. In mice with kidney and cardiac fibrosis, the ablation of these cells resulted in reduction in fibrosis and rescued heart function.
“We’ve found that these Gli1 progenitor cells differentiate into myofibroblasts, and in fibrotic disease, when they are ablated, we can rescue organs and organ function,” said Humphreys.
Researchers note that the genetic strategy employed in the preclinical model is not feasible in humans. For this reason, future research involves the exploration of drugs that could specifically target and shut off these fibrosis-causing stem cells with the hope that either an existing drug or a new drug could translate to a potential therapy for humans.
Humphreys also notes that this cell population plays a role in the aging process. “Most organs develop fibrosis as we age,” he said. “Specifically, in the kidney we lose one percent of kidney function as a result of fibrosis for each year that we age. We look forward to future research, using human tissue, to confirm our findings in humans and work to develop a potential therapy.”
This research was supported by the Harvard Stem Cell Institute, the National Institutes of Health, the National Institute of Diabetes and Digestive and Kidney Diseases, the American Heart Association, and the Deutsche Forschungsgemeinschaft.
Story Source:
The above story is based on materials provided by Brigham and Women’s Hospital. Note: Materials may be edited for content and length.
Journal Reference:
- Rafael Kramann, Rebekka K. Schneider, Derek P. DiRocco, Flavia Machado, Susanne Fleig, Philip A. Bondzie, Joel M. Henderson, Benjamin L. Ebert, Benjamin D. Humphreys. Perivascular Gli1 Progenitors Are Key Contributors to Injury-Induced Organ Fibrosis. Cell Stem Cell, 2014; DOI: 10.1016/j.stem.2014.11.004