A study of breast cancers detected with screening mammography found that strong family history and dense breast tissue were commonly absent in women between the ages of 40 and 49 diagnosed with breast cancer. Results of the study were presented today at the annual meeting of the Radiological Society of North America (RSNA).
“Screening recommendations for this age group continue to be debated,” said Bonnie N. Joe, M.D., Ph.D., associate professor in residence and chief of women’s imaging at University of California, San Francisco (UCSF). “Recent publications have suggested risk-based screening based on family history and breast density. However, our study shows that this approach would miss a significant percentage of invasive cancers and could potentially be dangerous.”
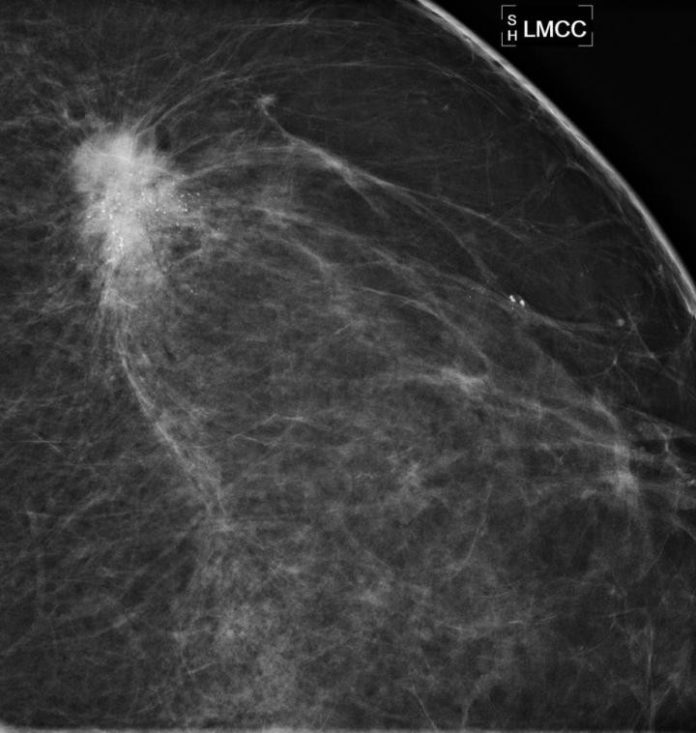
The retrospective study, conducted at UCSF, included 136 women between the ages of 40 and 49 with breast cancer identified by screening mammography between 1997 and 2012. Symptomatic patients undergoing diagnostic mammography and those with a personal history of breast cancer were excluded from the study. Patient family history, breast density, type of malignancy, lymph node status, and tumor receptor status were recorded.
“Notably, we found that almost 90 percent of the invasive cancers we would have missed using risk-based triage had positive receptor status, meaning they were very treatable and worth finding early,” Dr. Joe said.
Of the 136 breast cancer cases identified, 50 percent were diagnosed as invasive, and 50 percent were diagnosed as ductal carcinoma in situ (DCIS), an early noninvasive form of breast cancer, although 88 percent of DCIS cases were intermediate or high grade.
A very strong family history was absent in 90 percent of patients, and extremely dense breast tissue was absent in 86 percent. Seventy-eight percent of patients had neither strong family history nor extremely dense breasts, including 79 percent of the cases of invasive disease.
“Our results show that by exclusively using a risk-based approach to screening mammography, we could potentially miss more than 75 percent of breast cancers in women in their 40s, thereby eliminating most of the survival benefit from screening mammography that has been previously shown in randomized controlled trials,” Dr. Joe said.
Dr. Joe urges proponents of risk-based screening to continue research to find more effective means of risk-based triage.
“Neither family history nor breast density in combination or alone are sufficient risk factors to safely triage patients in risk-based screening,” she explained.
Routine annual screening mammography has traditionally been recommended by organizations such as the American Cancer Society (ACS) and the American Medical Association (AMA) for all women beginning at age 40. In 2009, the United States Preventive Services Task Force (USPSTF) issued controversial new guidelines recommending screening with mammography every two years beginning at age 50.
“Based on our current knowledge and evidence shown in previous trials, it is still safest to get annual mammograms starting at age 40 in order to maximize the survival benefit of screening mammography,” Dr. Joe said.
Story Source:
The above story is based on materials provided by Radiological Society of North America. Note: Materials may be edited for content and length.