An international team of scientists which includes researchers from the U. of Granada has demonstrated for the first time that it is possible to establish in an objective way the level of fatigue in physicians after long shifts through their eye movement.
This research reveals that the speed of saccadic movement (mostly voluntary rapid eye movements which we use to focus our gaze upon an object that attracts our attention) is an excellent index to measure objectively the level of fatigue in the medical profession.
In an article published in Annals of Surgery, scientists evaluated the performance of doctors from the Traumatology Service at St Joseph’s Hospital and Medical Centre, Phoenix (US), before and after their so called ‘call-day’ (a 24-hour shift during which doctors do not get any sleep)
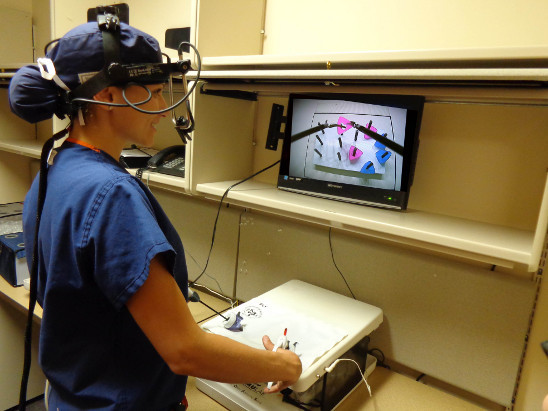
All of them had the speed of their saccadic eye movements measured before and after the shift. Besides, they had to perform simulated laparoscopic tests (also before and after this 24-hour shift)
Subjective fatigue perception
Results proved that after long hours, the speed of saccadic movements effectively diminished, while their subjective perception of fatigue increased. However, in the simulated laparoscopic tests after the shift, the execution was not affected in any significant way by their fatigue.
This means that — fortunately for patients — the previous work hours did not have a negative impact on their surgery practice. This supports the hypothesis that fatigue is not the only source of errors in medical professionals. Although shifts involve restless work, doctors, in their professional practice, always display all the resources available to obtain the best results. There is, for instance, a complex relation between continuous care, patient safety, economic factors, and the level of fatigue in doctors themselves.
“It is also true that those other professional competence resources can do little when there is an excess of working hours, and consequently those results are fundamental to contribute to the regulation of shifts and schedules, based on objective data on fatigue and performance,” suggested Leandro Luigi Di Stasi, Fulbright researcher at the Barrow Neurological Institute(Phoenix, AZ, US), and Andrés Catena, director of the Centre for Research on Mind, Brain and Behaviour at the University of Granada.
More than a decade ago, the U.S. Government’s National Institute of Medicine published a report titled “To Err Is Human: Building a Safer Health System”, which estimated that medical errors were responsible for between 44,000 and 98,000 deaths in the U.S., and more than a million injuries every year.
Although these estimates are not devoid of controversy, it is obvious that medical errors and accidental damage do occur too frequently. In particular, errors originating in fatigue have been identified as one of the factors that lead to most accidents at work. The costs of such accidents has been recently estimated to amount to 31,1 billion dollars in the U.S.
Avoiding errors
In Spain, around 10% of patients in hospital suffer some type of adverse episode as a result of medical attention, and about 50% of these errors could have been avoided by the application of safer clinical practices.
“For these reasons, all those strategies whose objective is to know the factors that lead to unsafe medical practices, and consequently diminish patient safety, are part of the agenda of several international organizations, including the World Health Organization,” according to Di Stasi and Catena.
Since long work shifts and overtime hours are both becoming more frequent, especially among resident doctors, “the study of fatigue as a factor that contributes to the prevention of errors in the health system has become one of the main topics in risk management within this context.”
The results of this research also open to debate the number of hours that doctors can work without affecting patient safety. For instance, in the U.S. residents work almost twice as their Spanish or French counterparts (80 hours a week vs 40)
The results of this study can also be applied to other fields similar to medicine, which also require long hours involving large amounts of sophisticated knowledge and complex decision-making skills coupled with technical complexity — such as civil and military aviation.
Story Source:
The above story is based on materials provided by University of Granada. Note: Materials may be edited for content and length.
Journal Reference:
- Leandro L. Di Stasi, Michael B. McCamy, Stephen L. Macknik, James A. Mankin, Nicole Hooft, Andrés Catena, Susana Martinez-Conde. Saccadic Eye Movement Metrics Reflect Surgical Residentsʼ Fatigue. Annals of Surgery, 2014; 259 (4): 824 DOI: 10.1097/SLA.0000000000000260