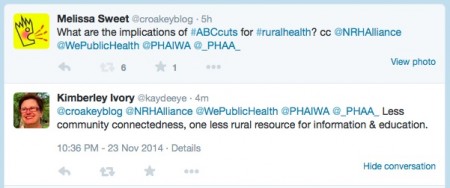
The ABC cuts announced today will have significant ramifications for the health and wellbeing of rural and regional communities, an issue that will be explored at Croakey in coming days (in the meantime, see some of the tweets at the bottom of this post).
Meanwhile, the wide-ranging impacts upon rural and remote communities of cuts to public dental services are investigated below by Anne-marie Boxall, Senior Policy Adviser at the National Rural Health Alliance.
This is the final article in Croakey’s recent rural health series.
***
Restoration of funding for public dental services is a rural health priority
Anne-marie Boxall writes:
In the Budget handed down in May this year, the Abbott Government deferred for a year the decision foreshadowed in the National Partnership Agreement on adult public dental services.
Under that Agreement the Commonwealth is to provide additional funding to State and Territory Governments for the provision of dental health services for low-income adults who rely largely on the public dental system.
The funding is now slated to begin in 2015-16 and the NRHA’s main purpose is to ensure that it is not postponed again.
The savings that will result from putting this Agreement on hold for a year (and those that come from cutting the Dental Flexible Grants Programme) were to be invested in the Medical Research Future Fund. However, legislation to establish that Fund has not yet been introduced, partly because it is contingent on funding from the Government’s $7 co-payment proposal.
No-one could reasonably oppose the idea of doing more health research, particularly if there is some prospect of finding answers for diseases and conditions which affect so many around the world.
However, worthy long-term causes should not drain resources from more urgent conditions which are almost entirely preventable and which are literally staring us in the face.
“Simply appalling”
The state of oral and dental health among disadvantaged groups in Australia is simply appalling and a poor reflection on a health service which is otherwise good by international standards. Those disadvantaged groups include people on low incomes, many Aboriginal and Torres Strait Islander people, and those in more remote areas who find themselves at a distance from fee-for-service oral health care.
The NRHA is strongly opposed to the government making savings of $390 million over four years at the expense of those who are in discomfort, may be admitted to hospital by default, may not be able to eat properly and fear the act of smiling. And it will be strongly opposed to any suggestion that these funds should be diverted to health research.
It should be remembered that, on average, people in rural and remote areas have lower incomes than those in the major cities. This means their access to timely oral health care is compromised by both income and access.
At the NRHA’s CouncilFest in September its 37 member bodies agreed to make the restoration of funding for public dental services a priority issue for the year ahead. Here are some of the reasons why.
People in rural and remote areas have poorer oral health than their city counterparts. The proportion of people with untreated decay, for example, increases with remoteness (see Tables 2.9 of this report from the Australian Institute of Health and Welfare (AIHW)). People in more remote areas also have higher rates of gum disease (see Table 2.3 in this AIHW report).
In 2011 there were 64.1 full-time equivalent (FTE) dentists per 100,000 people in major cities, but only 33.5 in outer regional areas and 26.4 in remote or very remote areas (see here for data tables).
The trend is similar for dental hygienists: 4.4 FTE per 100,000 in major cities, but the rate is 0.3 in remote or very remote areas. There are more dental therapists per head outside major cities but they largely work with children so they cannot remedy access problems for adults.
Limited access to services
Access to dental care in rural areas is also limited in some areas because rates of private insurance (that include dental cover) are much lower than they are in major cities.
Data from the AIHW shows the proportion of people with dental insurance in major cities in 2010 was 59.2 per cent, whereas it was 47.0 per cent in inner regional and 46.3 per cent in outer regional areas. Insurance rates in remote and very remote areas were lower than in major cities (55.7 per cent), but higher than in other non-metropolitan areas.
Insurance rates are important because so much dental care is provided in the private sector, and private insurance provides some protection against high out-of-pocket costs.
Given the lower rates of insurance in rural Australia, it is not surprising that reliance on public dental services is higher in rural and remote areas.
These data from the AIHW (see Table 4.11) show that the proportion of people using public dental services in 2010 in inner and outer regional areas was 8.3 and 8.6 per cent, respectively; the proportion in major cities was lower at 5.1 per cent. These public services are the ones adversely affected by the decision to defer the National Partnership Agreement.
The additional resources to be invested through the National Partnership Agreement would be directed at the public oral health sector, but could be out-sourced to private practitioners.
Around 90 per cent of dental care is provided in the private sector and even with the proposed extra resources, the public sector will not have the capacity any time soon to provide all that is needed by under-served populations and in under-served regions.
A social and economic concern
Improving dental health for people in the bush is an important issue in its own right, but the Alliance has taken up the fight because it recognises the broader significance of good oral health on people’s overall health, and on their social, economic and emotional wellbeing.
It is well known that there is a link between dental diseases and other health conditions.
Periodontal disease for example is linked to heart disease, and people in rural areas already suffer disproportionately from cardiovascular disease.
Recently released data from the National Heart Foundation shows that people living in regional and rural Australia have a 26 per cent greater risk of cardiovascular disease than those in major cities (see here for a map illustrating prevalence across Australia).
Australian researchers have found evidence of the links between oral health and general wellbeing. One study, for example, has shown that there is a relationship between poor oral health and anxiety and depression in young Aboriginal women.
Conversely, the study found a relationship between resilience in young Aboriginal men and owning a toothbrush and having cavities filled. This research suggests that the pay-offs for improving oral health go well beyond the mouth.
Economic impacts
Dental problems also have a direct impact on the economy. Research shows that in 2010, 9 per cent of adults missed one half day or more from paid work or study due to dental problems.
Overall, this equated to approximately 2.4 million occasions where people took half a day or more off work or study. The estimated cost to the economy in lost productivity was thought to be approximately $453 million annually.
The health sector, including the NRHA, recognises the need for Australia to tighten its belt and make sure government funds are spent as wisely as possible. However, cutting funding for public dental services is a false economy.
By failing to address the inequalities in access to services and dental health outcomes for people in rural and remote Australia now, we will only increase health and economic costs over the longer term.
Poor oral health is almost entirely preventable. Whether the focus is economic productivity, good health or simple old-fashioned fairness, one of the best investments is in public oral health services.
And, assuming that an appropriate workforce is provided, the people living in the communities of rural and remote Australia will be among the main beneficiaries.
Rural people will be watching next May’s Budget very carefully – their mouths wide open in anticipation.
***
Previous articles in the series, which was inspired by the NRHA’s recent CouncilFest:
- Love rural? What WAS that all about…
- Deregulation of university fees: bad news for rural people and regional universities?
- The rural health risks of the transition to Primary Health Networks
- Improving broadband
***
Meanwhile, on the ABC cuts and rural health