Patients with hip and knee osteoarthritis may improve their pain, stiffness and physical function with sustained physical exercise, manual therapy or both, according to new research findings presented this week at the American College of Rheumatology Annual Meeting in Boston.
Osteoarthritis, or OA, is the most common joint disease affecting middle-age and older people. It is characterized by progressive damage to the joint cartilage — the cushioning material at the end of long bones — and causes changes in the structures around the joint. These changes can include fluid accumulation, bony overgrowth, and loosening and weakness of muscles and tendons, all of which may limit movement and cause pain and swelling.
Existing evidence supports the effectiveness of exercise and manual therapy for easing hip and knee OA symptoms and improving physical function. However, no data existed to compare the addition of these treatment approaches to usual medical care for OA or for the long-term efficacy of this holistic approach. Researchers in New Zealand studied 206 OA patients for two years to measure the efficacy of adding regular physical exercise, manual therapy, or a combination of both therapies to standard care, versus continuing usual medical care for OA alone.
“The aim of this study was to establish whether providing a comprehensive program of exercise or manual therapy results in significant additional benefits, over and above usual medical care,” said J. Haxby Abbott, DPT, PhD, FNZCP at the University of Otago in Dunedin, New Zealand, and a lead author on the study.
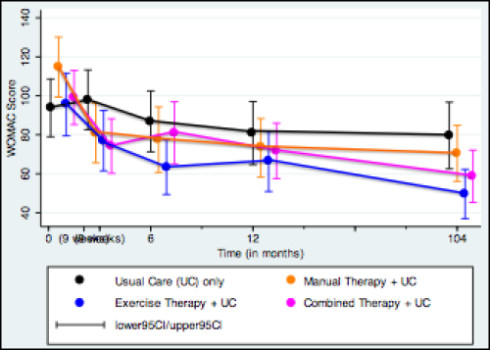
The participants’ progress was measured using the Western Ontario and McMaster (WOMAC) OA index, which calculates scores on a scale of 0-240. Lower WOMAC scores indicate improvements in pain, stiffness and physical function. Participants were also given several physical performance tests -Timed up-and-go, 40-meter fast-paced walk and a 30-second sit-to-stand. At baseline, the mean age of the OA patients in the study was 66 years with a mean WOMAC score of 100.8.
After two years, all the participants who engaged in either regular exercise, manual therapy or a combination of both showed improved WOMAC scores that were superior to those who had only the usual medical care for OA.
Participants receiving exercise therapy in addition to their usual care showed improvement of 31.7 WOMAC points compared to usual care alone. Participants receiving manual therapy in addition to their usual care showed a relative improvement of 30.1 WOMAC points. While the difference in WOMAC improvement for participants receiving combined exercise therapy and manual therapy in addition to usual care did not meet the a priori threshold for clinical significance (28 points), there was a trend towards benefit, with this group improving 26.2 WOMAC points more than usual care only. Those participants in the exercise therapy group showed greater mean changes on most physical performance tests than anyone in the other groups.
Adding either exercise therapy or manual therapy to usual medical care is beneficial for people with hip and knee OA, the study’s authors concluded. “This study showed that benefits imparted by a comprehensive program of exercise therapy or manual therapy, provided by Physical Therapists, remain significant to at least two years follow-up,” said Dr. Abbott.
Story Source:
The above story is based on materials provided by American College of Rheumatology (ACR). Note: Materials may be edited for content and length.