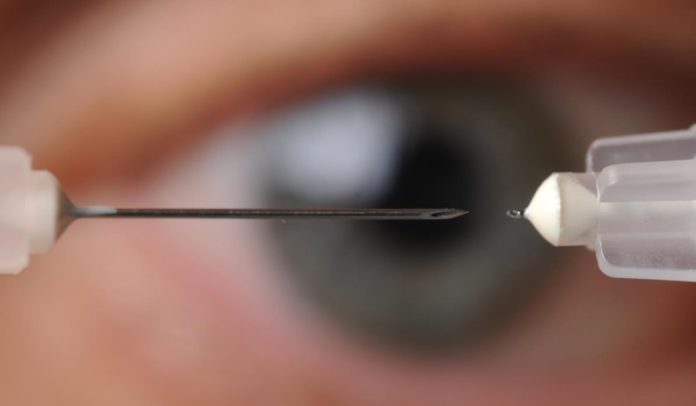
Needles almost too small to be seen with the unaided eye could be the basis for new treatment options for two of the world’s leading eye diseases: glaucoma and corneal neovascularization.
The microneedles, ranging in length from 400 to 700 microns, could provide a new way to deliver drugs to specific areas within the eye relevant to these diseases. By targeting the drugs only to specific parts of the eye instead of the entire eye, researchers hope to increase effectiveness, limit side effects, and reduce the amount of drug needed.
For glaucoma, which affects about 2.2 million people in the United States and is the second leading cause of blindness worldwide, the goal is to develop time-release drugs that could replace daily administration of eye drops. A painless microneedle injection made once every three to six months – potentially during regular office visits – could improve treatment outcomes by providing consistent dosages, overcoming patient compliance issues.
In the second disease, corneal neovascularization, corneal injury results in the growth of unwanted blood vessels that impair vision. To treat it, the researchers developed solid microneedles for delivering a dry drug compound that stops the vessel growth.
“The power of microneedles for treating eye conditions is the ability to target delivery of the drug within the eye,” said Mark Prausnitz, a Regents’ professor in the School of Chemical and Biomolecular Engineering at the Georgia Institute of Technology. “We are developing different microneedle-based systems that can put the drug precisely into the part of the eye where it’s needed. In many cases, we hope to couple that delivery with a controlled-release formulation that would allow one application to treat a condition for weeks or months.”
The research, which was supported by the National Eye Institute of the National Institutes of Health (NIH), was reported November 13 in the journal Investigative Ophthalmology & Visual Science. The research was done using animal models, and could become the first treatment technique to use microneedles for delivering drugs to treat diseases in the front of the eye.
Glaucoma results from elevated pressure inside the eye that can be treated by reducing production of the aqueous humor fluid in the eye, increasing flow of the fluid from the eye, or both. Glaucoma is now controlled by the use of eye drops, which must be applied daily. Studies show that as few as 56 percent of glaucoma patients follow the therapy protocol.
The microneedle therapy would inject drugs into space between two layers of the eye near the ciliary body, which produces the aqueous humor. The drug is retained near the injection side because it is formulated for increased viscosity. In studies with an animal model, the researchers were able to reduce intraocular pressure through the injections, showing that their drug got to the proper location in the eye.
Because the injection narrowly targets delivery of the drug, researchers were able to bring about a pressure reduction by using just one percent of the amount of drug required to produce a similar decline with eye drops. The research team, which also included Georgia Tech postdoctoral fellow Yoo Chun Kim and Emory University Emeritus Professor of Ophthalmology Henry Edelhauser, hopes to produce a time-release version of the drug that could be injected to provide therapy lasting for months.
“The ultimate goal for us would be for glaucoma patients visiting the doctor to get an injection that would last for the next six months, until the next time the patient needed to see the doctor,” said Prausnitz. “If we can do away with the need for patients to use eye drops, we could potentially have better control of intraocular pressure and better treatment of glaucoma.”
To treat corneal neovascularization, the researchers took a different approach, coating solid microneedles with an antibody-based drug that prevents the growth of blood vessels. They inserted the coated needles near the point of an injury, keeping them in place for approximately one minute until the drug dissolved into the cornea.
In an animal model, placement of the drug halted the growth of unwanted blood vessels for about two weeks after a single application. In addition to the researchers already mentioned, the corneal neovascularization research included Emory University Professor of Ophthalmology Hans Grossniklaus.
While the research reported in the journal did not include time-release versions of the drugs, a parallel project is evaluating potential formulations that would provide that feature.
Eye injections with hypodermic needles much larger than the microneedles are routinely used to administer compounds into the center of eye. These injections are well tolerated, and Prausnitz expects the use of microneedles would also not cause significant side effects.
“Increasingly, eye drops are not able to deliver drugs where they need to go, so injections into the eye are becoming more common,” said Edelhauser. “But hypodermic needles were not designed for the eye and are not optimal for targeting drugs within the eye.”
In contrast to the larger hypodermic needles, the microneedles are tailored to penetrate the eye only as far as needed to deliver the drugs to internal spaces within the layers of the eye. For the glaucoma drug, for instance, the needle is only about half a millimeter long, which is long enough to penetrate through the sclera, the outer layer of the eye, to the supraciliary space.
Both potential treatments would require additional animal testing before human trials could begin.
Story Source:
The above story is based on materials provided by Georgia Institute of Technology. The original article was written by John Toon. Note: Materials may be edited for content and length.
Journal Reference:
- M. R. Prausnitz, Y. C. Kim, H. E. Grossniklaus, H. F. Edelhauser. Intrastromal delivery of bevacizumab using microneedles to treat corneal neovascularization. Investigative Ophthalmology & Visual Science, 2014; DOI: 10.1167/iovs.14-15257