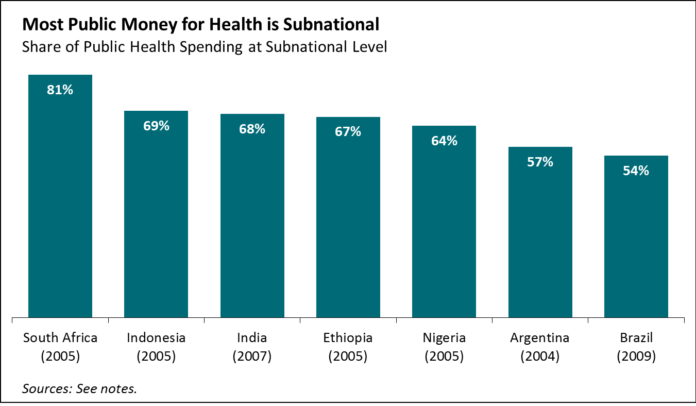
In the big federal countries where global disease burden is concentrated, most public money for health isn’t ultimately spent by the national ministry of health, the traditional counterpart for global health funders and technical agencies. Instead, most money is programmed and spent subnationally (see figure 1).

Greater subnational public spending reflects growing democratization and local self-determination, particularly in middle-income countries, and responds to the conviction that local decision-makers understand local realities better than a bureaucrat sitting in the capital city. Yet evidence on the effectiveness of subnational spending on health is mixed, and incentives for greater spending, better performance, and enhanced accountability can be weak.
As more donors hope for greater levels of domestic funding for global health priorities in middle-income countries, it’s important to know how well that money is being spent. We took a look at whether allocations of public money to subnational jurisdictions are done according to need, whether they create incentives for better performance or more spending on health, and whether they generate accountability for spending and results. The results of our analysis inform the consultation draft of “Intergovernmental Fiscal Transfers for Health: Overview Framework and Lessons Learned” (comments welcome by December 15), which intends to trigger a rethink on how governments and donors engage to achieve health goals.
Our draft is rich in detail but boils down to four key messages:
- Allocation can but doesn’t usually track to need. In India, spending in Bihar, the state with the lowest per capita health spending, is less than half of the spending in Kerala and Tamil Nadu, and gaps between states widened as the health system became more decentralized. Although India uses a formula to allocate according to need, it uses 1971 as the base year for the population estimates in the formula. Similarly, in Nigeria, the urban-rural divide in terms of health service delivery deteriorated after states obtained more responsibility and spending power. But there are better examples: in Punjab, Pakistan, the province shifted from an input-based budget for districts to a “performance-based equitable resource allocation model” that has resulted in more progressive allocation of monies, though an evaluation by the World Bank is ongoing.
- Incentives matter. Subnational entities may decrease their own spending if they get more money from the national government (or donors). Under pre-Modi reforms in India, states actually decreased their own health spending when more money was earmarked for health from the central government. Similarly, in China, many poor states do not match federal matching grants with their own budgets. Last week, we posted on the dilemmas facing Nigeria’s TB program when states receive basket funds for health but few incentives for increased fiscal effort or better TB outcomes. Such concerns have long been on the agenda in the aid effectiveness dialogue on the fungibility and additionality of funding, but are even more important as external funders such as PEPFAR, GAVI, and the Global Fund call for more domestic spending on global health priorities (AIDS, TB, vaccination). In contrast, the US Medicaid program creates incentives for greater state government funding by matching state contributions dollar for dollar, resulting in larger state allocations to health.
- Design matters. There’s mixed evidence on whether conditions attached to fiscal transfers between levels of government have worked to improve performance. South Africa, for example, has been implementing conditional grants to subnational entities geared toward HIV/AIDS treatment and prevention, school nutrition, basic education, and infrastructure programs, but these grants are not conditioned on easily measurable outcomes and do not link policy and budgets. In contrast, Argentina through Plan Nacer has used conditional grants to incentivize provinces to expand coverage of maternal and child health interventions, using a strengthened provincial level information system as well as an external audit and impact evaluation to assess the level of compliance with conditionality. Plan Nacer’s impact evaluation results suggest a large and significant increase in service coverage and a large decline in the neonatal mortality rate among beneficiaries.
- Few countries have adequate systems for financial or performance accountability in place; this requires greater attention. The World Bank’s Country Policy and Institutional Assessment (CPIA) rates countries on the quality of budgetary and financial management, among other measures. Of the 80 or so World Bank International Development Association (IDA) borrowing countries, none attain a 5 or greater (0–6 scale). The measures include the ability at the national level to report expenditures and audit findings in a timely matter and public access to annual budget documentation, suggesting that the most basic accountability may not be in place for policymakers to do their jobs. Recent experience suggests that greater investment in public financial management can yield results: SIGFE in Angola (PDF) and e-SISTAFE in Mozambique being examples. Nascent efforts to benchmark state performance on effective coverage in Mexico aimed to foster greater competition and transparency among states, but also led to states refusing to report and federal authorities with little leverage to force compliance. Citizen watchdogging holds promise but is also limited by the lack of data on spending and service provision. Evidence is still mixed on its effectiveness.
- There are missed opportunities to act on lessons and learn from reforms. The multilateral development banks have long been engaged in this area, but too frequently the fiscal people don’t talk to the health people, and we see missed opportunities to improve health in key countries like India, Indonesia and the Philippines, among others. The IMF’s Government Finance Statistics doesn’t even report subnational spending by sector such that analysts could evaluate the effects of fiscal transfers. Further, inter-governmental fiscal transfers remain under-researched and under-invested; even after reforms, governments (and their funding partners) know little about whether a new allocation formula changed the distribution of spending or whether conditions attached to transfers generated improvements in service delivery or health status. In our review, we found few rigorous evaluations and the exception focused on conditional block grants through the aid system rather than the fiscal system! (though an excellent study, see here)
What does it all mean for donors and advocates?
Whether a donor or advocate cares most about increasing spending on AIDS or child health in middle-incomes and assuring a smooth “transition” from aid, or whether focused on health systems and UHC, the plumbing involved in a country’s system of inter-governmental fiscal transfers merits a closer look. Opportunities to act on lessons learned and learn from on-going reforms should be seized, and more systematic joint learning with country policymakers, as well as a policy and learning agenda should be launched.
What more can be done? We hope you’ll check out the consultation draft of the lessons learned paper that includes examples where countries successfully improved health outcomes through better practices. We welcome your comments by the end of the year. And watch for papers and working group reports from our collaboration with India’s Accountability Initiative on the same topic.
Sources for Figure 1:
- South Africa: IMF Government Finance Statistics (2011)
- Indonesia: World Bank (2008). Investing in Indonesia’s Health: Challenges and Opportunities for Future Public Spending – Health Public Expenditure Review 2008. Washington DC, World Bank
- India: IMF Government Finance Statistics (2011)
- Ethiopia: Garcia, M. and A. S. Rajkumar (2008). Achieving Better Service Delivery Through Decentralization in Ethiopia. World Bank Working Papers. Washington DC, World Bank
- Nigeria: Olaniyan, O. and A.O. Lawanson (2010). Health Expenditure and Health Status in Northern and Southern Nigeria: A Comparative Analysis Using NHA Framework. Paper presented at the 2010 CSAE conference held at St. Catherine’s College, University of Oxford, Oxford, UK
- Argentina: IMF Government Finance Statistics (2011)
- Brazil: Langevin, M. (2012). Brazil’s Healthcare System: Towards Reform? A BrazilWorks Briefing. Washington DC, BrazilWorks
- Bolivia: IMF Government Finance Statistics (2011)