Glycogen storage disorders, which affect the body’s ability to process sugar and store energy, are rare metabolic conditions that frequently manifest in the first years of life. Often accompanied by liver and muscle disease, this inability to process and store glucose can have many different causes, and can be difficult to diagnose. Now, researchers at the University of Missouri who have studied enzymes involved in metabolism of bacteria and other organisms have catalogued the effects of abnormal enzymes responsible for one type of this disorder in humans. Their work could help with patient prognosis and in developing therapeutic options for this glycogen storage disease.
“In February of this year, I found an article in the New England Journal of Medicine (NEJM) that caught my eye,” said Lesa Beamer, associate professor of chemistry and biochemistry at MU. “It was a landmark study identifying a new, inherited metabolic disorder in humans called phosphoglucomutase 1 (PGM1) deficiency, and affects the human versions of the very same enzymes I had studied.”
The NEJM study was the first to characterize the multiple effects of the disorder in humans and pinpointed the enzyme involved. The disorder, described initially in 21 patients, is considered rare but will likely be found more often now that genetic tests have been developed. According to the study, the disease often affects patients in early childhood or adolescence, and can cause hypoglycemia, muscle disease, hormonal abnormalities, and cardiac problems. Many patients exhibit exercise intolerance and, because the condition could not previously be diagnosed, these problems sometimes led to early deaths.
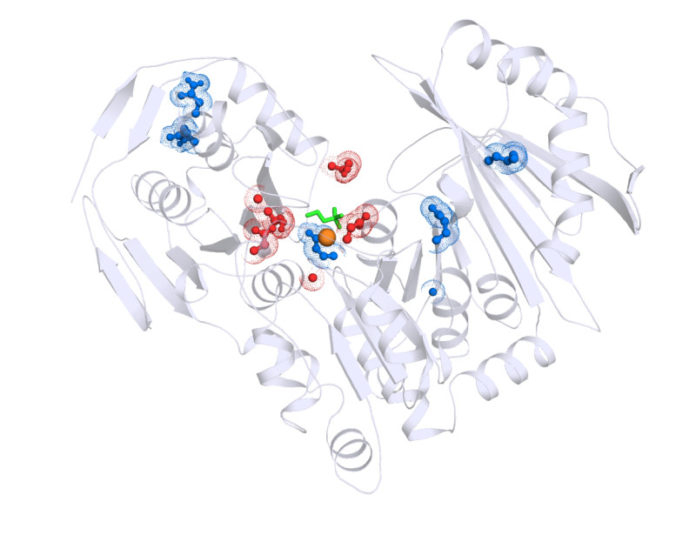
Beamer’s lab researches similar enzymes in bacteria that play important roles in carbohydrate (sugar) metabolism, including sugars like glucose. These enzymes perform the same chemical reaction as the human protein involved in the newly identified inherited disease, and share many other similarities.
“Once the disease involving the human equivalent had been identified, we were able to put the knowledge we’ve gained to immediate use,” Beamer said. “Using the information provided by the NEJM study, we recreated the mutated proteins that cause the disorder in a test tube, and conducted detailed biochemical analyses. Our study was the first to systematically characterize and index these mutant proteins for comparison with the symptoms in human patients. Because patient studies are complex and time-consuming, our biochemical analyses are proving essential to understanding the complicated clinical presentation of this inherited disorder.”
The early-stage results of this research are promising. If additional studies are successful, Beamer believes that her bacterial enzyme research could assist with further research studying the development of human genetic health tests and therapeutics within the next few years. Her lab currently is collaborating with human medical researchers to “fast track” the study of this rare disease.
Story Source:
The above story is based on materials provided by University of Missouri-Columbia. Note: Materials may be edited for content and length.
Journal Reference:
- Y. Lee, K. M. Stiers, B. N. Kain, L. J. Beamer. Compromised catalysis and potential folding defects in in vitro studies of missense mutants associated with hereditary phosphoglucomutase 1 deficiency. Journal of Biological Chemistry, 2014; DOI: 10.1074/jbc.M114.597914