McLean Hospital and Harvard Stem Cell Institute scientists have new evidence that stem cell transplantation could be a worthwhile strategy to help epileptics who do not respond to anti-seizure drugs.
As reported in Cell Stem Cell, the laboratory of McLean Associate Neurobiologist Sangmi Chung, PhD, transplanted seizure-inhibiting, human embryonic stem cell-derived neurons into the brains of mice with a common form of epilepsy. Half of the mice who received the transplanted neurons no longer had seizures, while the other half experienced a significant drop in seizure frequency.
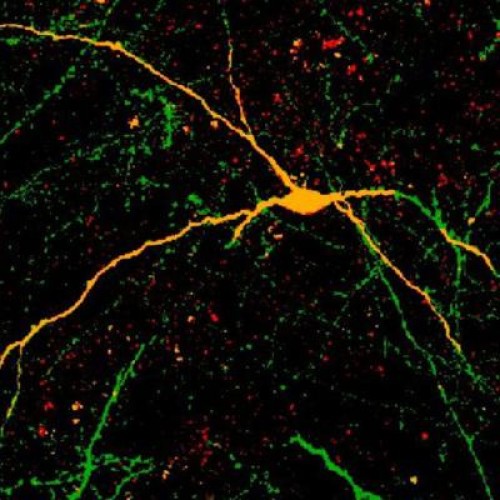
“After the transplantation we observed that the human neurons integrate into the epileptic brain,” said Chung, who is also a Harvard Stem Cell Institute affiliated faculty member and an assistant professor at Harvard Medical School. “The transplanted neurons begin to receive excitatory input from host neurons and in turn generate inhibitory responses that reverse the electrical hyperactivity that cause seizures.”
The recovery seen after the human stem cell-derived neuron transplants, which were done while the cells were still maturing into their full-grown form, is similar to that published in a 2013 study by University of California, San Francisco, scientists who transplanted fetal mouse brain cells into epileptic mice.
While encouraging, Chung noted that further primate studies and a process to purify the neurons, so only those known to inhibit seizures are transplanted (called interneurons), would need to be completed before a treatment in humans could be considered.
“Because embryonic stem cells can differentiate into many different cell types, even when we drive them into neurons, there are always other cell types,” she said. “For clinical purposes, we need to make sure the cells are safe, without any contaminant. Currently we are working on a different method to specifically isolate interneurons.”
Over 65 million people worldwide are affected by epileptic seizures, which can cause convulsions, loss of consciousness and other neurological symptoms. The exact cause of the condition is unknown, but it is hypothesized that diminished populations of interneurons is a contributor.
Most epileptic patients can be treated with anti-seizure drugs, which contain molecules that can inhibit electrical symptoms, similar to the normal function of interneurons. But about one-third do not benefit from existing medication. Patients may opt to have a portion of their brain cut out to control symptoms.
“This seems to be an area that needs a novel therapy,” Chung said. “Before starting this project, I was a stem cell biologist mostly interested in the development of neural stem cells, but as I’ve come to know about epilepsy, I’ve become motivated to continue this research.”
Story Source:
The above story is based on materials provided by McLean Hospital. The original article was written by Adriana Bobinchock. Note: Materials may be edited for content and length.
Journal Reference:
- Miles Cunningham, Jun-Hyeong Cho, Amanda Leung, George Savvidis, Sandra Ahn, Minho Moon, Paula K.J. Lee, Jason J. Han, Nima Azimi, Kwang-Soo Kim, Vadim Y. Bolshakov, Sangmi Chung. hPSC-Derived Maturing GABAergic Interneurons Ameliorate Seizures and Abnormal Behavior in Epileptic Mice. Cell Stem Cell, 2014; 15 (5): 559 DOI: 10.1016/j.stem.2014.10.006