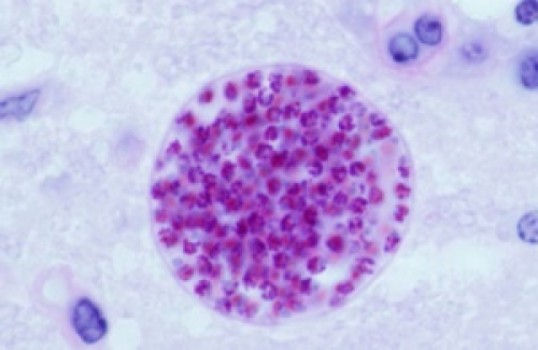
Many factors, both genetic and environmental, have been blamed for increasing the risk of a diagnosis of schizophrenia. Some, such as a family history of schizophrenia, are widely accepted. Others, such as infection with Toxoplasma gondii, a parasite transmitted by soil, undercooked meat and cat feces, are still viewed with skepticism.
A new study by Gary Smith, professor of population biology and epidemiology at the University of Pennsylvania’s School of Veterinary Medicine, used epidemiological modeling methods to determine the proportion of schizophrenia cases that may be attributable to T. gondii infection. The work, published in the journal Preventive Veterinary Medicine, suggests that about one-fifth of cases may involve the parasite.
“Infection with Toxoplasma is very common, so, even if only a small percentage of people suffer adverse consequences, we could be talking about problems that affect thousands and thousands of people,” Smith said.
In the United States, just over a fifth of the population is infected with T. gondii. The vast majority aren’t aware of it. But there are some populations that need to be concerned. For example, if a woman becomes infected for the first time during pregnancy, her fetus can die or suffer serious developmental problems. People with HIV or other diseases that weaken the immune system are susceptible to a complication of T. gondii infection called toxoplasmic encephalitis, which can be deadly.
Though the medical community has long believed that most healthy people suffer no adverse effects from a T. gondii infection, recent studies have found evidence of worrisome impacts, including an association with schizophrenia because the parasite is found in in the brain as well as in muscles. Other work has shown that some antipsychotic drugs can stop the parasite from reproducing. In addition, field and laboratory studies in mice, rats and people have shown that infection with T. gondii triggers changes in behavior and personality.
To further investigate this connection, Smith sought to calculate the population attributable fraction, or PAF, a metric epidemiologists use to determine how important a risk factor might be. In this case, Smith explained that the PAF is “the proportion of schizophrenia diagnoses that would not occur in a population if T. gondii infections were not present.”
The usual method of calculating the PAF was not well suited to examining the link between schizophrenia and T. gondii, because some of the variables are constantly in flux. For example, the proportion of people infected by T. gondii increases with age. Using a standard epidemiological modeling format, but taking into account all of the age-related changes in the relevant factors, Smith found the average PAF during an average lifetime to be 21.4 percent.
“In other words, we ask, if you could stop infections with this parasite, how many cases could you prevent?” Smith said. “Over a lifetime, we found that you could prevent one-fifth of all cases. That, to me, is significant.”
Smith noted that in some countries, the prevalence of T. gondii infection is much higher than in the U.S., and these countries also have a higher incidence of schizophrenia.
People with schizophrenia have greatly reduced life expectancies, and many are unable to work. Family members may also leave the workforce to care for relatives with the disease. For these reasons and others, schizophrenia acts as a large drain on the economy, responsible for $50 to $60 billion in health-care expenditures in the U.S. each year.
“By finding out how important a factor T. gondii infection is, this work might inform our attitude to researching the subject,” Smith said. “Instead of ridiculing the idea of a connection between T. gondii and schizophrenia because it seems so extraordinary, we can sit down and consider the evidence. Perhaps then we might be persuaded to look for more ways to reduce the number of people infected with Toxoplasma.”
The study was supported by the University of Pennsylvania School of Veterinary Medicine.
Story Source:
The above story is based on materials provided by University of Pennsylvania. Note: Materials may be edited for content and length.
Journal Reference:
- Gary Smith. Estimating the population attributable fraction for schizophrenia when Toxoplasma gondii is assumed absent in human populations. Preventive Veterinary Medicine, 2014; DOI: 10.1016/j.prevetmed.2014.10.009