Breast cancer screening, including routine mammography, has long been considered the gold-standard for risk assessment, but such screening can sometimes produce inconsistent results. But according to a new study from Stanford Medicine, genomic sequencing could be useful for identifying women who are most likely to benefit from screening, and it could also offer women a chance to reduce their risk of breast cancer.
The team, led by Dr. Alice Whittemore of the Department of Health Research and Policy at Stanford Cancer Institute in California, published their findings in the journal Cancer Epidemiology, Biomarkers & Prevention.
Breast cancer is the second leading cause of death among American women, behind lung cancer. This year, an estimated 232,670 women will be diagnosed with invasive breast cancer and 40,000 will die from the disease.
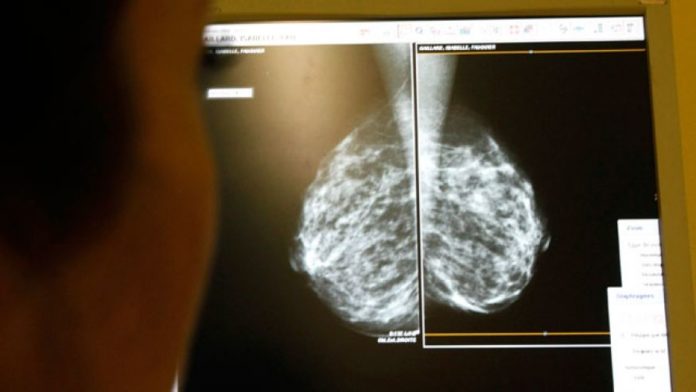
Since 1989, however, death rates from breast cancer have been declining. According to the American Cancer Society, this is partly due to earlier detection through screening, which in turn leads to earlier treatment and better treatment response. The most common breast cancer screening method is mammography, in which an X-ray of the breast is taken to check for tumors that may be too small to detect through a clinical breast exam. The test may also detect abnormal cells that pose a risk for invasive breast cancer.
But such screening methods are not flawless. A mammography, for example, can show false-negative results, meaning a woman who has breast cancer may fail to undergo treatment because her results appear normal. On the other hand, screening may produce false-positive results, meaning a woman may be subject to further examination or treatment for no reason; this is far more common than false-negative results. For instance, a study published just last month found that mammography may do more harm than good among older women (over the age of 70).
“We need low-cost screening tools that can discriminate between women who will and won’t develop fatal breast cancer that are more effective than those currently available,” says Dr. Whittemore.
Genomic sequencing ‘more effective for disease prevention than previously thought’
As such, the team looked to genomic sequencing, a process in which specific genes linked to certain diseases can be identified through searching small sections of DNA. Notably, past research has suggested that this process – which also involves ranking genes by risk and targeting genes that present high risk – would not be an effective breast cancer prevention technique. But this latest study challenges those claims.
After analyzing previously published data on 86 breast cancer gene variants known to be linked to breast cancer risk, the team created a computational model to estimate a woman’s lifetime risk of developing breast cancer. This was done by calculating a risk score, which is the number of breast cancer-related genetic variants a woman has multiplied by the effects of these variants.
The team found that based on the 86 breast cancer gene variants, the lifetime risk for the entire female population stood at 0.35, significantly higher than the 0.07 variance the researchers say was identified in a previous study. The researchers believe these findings indicate that genomic sequencing has the potential to effectively predict a woman’s risk of breast cancer.
“Our estimates suggest that preventive strategies based on genome sequencing will bring greater gains in disease prevention than previously projected,” says Dr. Whittemore. “Moreover, these gains will increase with increased understanding of the genetic etiology of breast cancer.”
The authors note that, as our knowledge of these genetic variants increases, their potential for use in breast cancer prevention will become even stronger. “As we keep identifying additional breast cancer variants that can further explain the difference between my risk versus yours, the variance of the genetic risk score in the population will increase, and the potential utility of genomic sequencing will grow,” says first author Dr. Weiva Sieh, assistant professor and epidemiologist at Stanford Cancer Institute.
But the potential implications extend beyond screening, as well, Dr. Sieh adds. “Our ability to predict the probability of disease based on genetics is the starting point. If a girl knew, from birth, what her inborn risk was, she could then make more informed choices to alter her future risk by altering her modifiable factors, such as diet and lifestyle.”
Latest developments in breast cancer screening
These findings are the latest in a string of recent discoveries aimed at improving breast cancer screening and detection methods.
In June, a study published in JAMA found that the addition of tomosynthesis, a 3D imaging technique, to digital mammography reduced the number of unnecessary callbacks and increased the rate of breast cancer detection. Digital tomosynthesis is a relatively new imaging technique that was only approved by the US Food and Drug Administration (FDA) in 2011 and has yet to become widely available.
Tomosynthesis aims to address the problems associated with traditional mammography by taking multiple X-ray pictures from different angles. The breast is positioned as it is for a conventional mammogram, but only a small amount of pressure is applied. The information is used to produce 3-D images throughout the entire breast, instead of a single one that conventional mammograms do.
To test the potential benefits of tomosynthesis, researchers compared screening results from 454,850 examinations, of which 173,663 utilized a combination of digital mammography and tomosynthesis, while the rest used only mammography. The results showed that the addition of tomosynthesis was associated with an decrease in the number false callbacks and an increase in the positive predictive value — the number of patients found to have breast cancer.
Another new screening technique, called ultrasound elastrography, also shows promise in early research. However, because the technique involves more complex imaging, results of ultrasound elastrography are vulnerable to misinterpretation. To address that problem, scientists have recently designed a virtual breast to help medical practitioners gain valuable experience interpreting results in the safety of the lab.
The virtual breast was developed using data from the Visible Human Project, which gathered thousands of cross-sectional photos from a female cadaver. Thus, it mimics the intricacy of the real thing, incorporating a variety of tissue types and anatomical structures, such as ligaments and milk ducts. Clinicians can practice looking for cancer by applying virtual ultrasound elastography to the virtual breast and then evaluating the resulting images. The scientists behind the project hope that the lab software will eventually be available to anyone who needs the training.
The latest findings from the Stanford team are sure to add to the ongoing debate over the effectiveness of mammography and its role in breast cancer prevention. While this debate has existed for years, the finding that has sparked the most debate recently was a 2012 study, published in the New England Journal of Medicine, which found that while mammography led to more treatment earlier, it didn’t necessarily save lives:
“Despite substantial increases in the number of cases of early-stage breast cancer detected, screening mammography has only marginally reduced the rate at which women present with advanced cancer. Although it is not certain which women have been affected, the imbalance suggests that there is substantial overdiagnosis, accounting for nearly a third of all newly diagnosed breast cancers, and that screening is having, at best, only a small effect on the rate of death from breast cancer.”