Many thanks to the Australian Commission on Safety and Quality in Health Care for these insights from the recently published OECD study on geographic variations in health care.
In May 2014, the Australian Commission on Safety and Quality in Health Care (the Commission) released a discussion paper on how provision of common hospital procedures varies across Australia (a Croakey piece on that work is here). The results suggested that the clinical management of patients with the same health conditions or concerns may depend on where they live or which health service they visit.
The work was part of an international project by the Organisation for Economic Cooperation and Development (OECD). A report comparing the results of all 13 participating countries was recently released.
How do Australian results compare?
For some procedures, Australian aggregate rates sit above the OECD average, while for others results are on par.
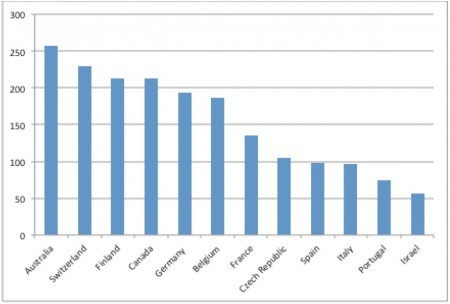
Australia’s aggregate knee replacement rate (more than 250 per 100,000 population) was the highest of the participating countries (Figure 1).
Figure 1: Standardised knee replacement rates (per 100,000 population) for selected OECD countries, 2011 or latest year
Source: OECD
Australia also had a relatively high hysterectomy rate (330 per 100,000 women). While Australian caesarean section rates were comparatively high (more than 340 per 1,000 live births), regional variation within Australia for caesarean section was the lowest of all the procedures examined.
Overall, the largest regional variation within, and between, the participating countries was observed in:
- cardiac procedures (angiography, coronary angioplasty and stenting, and heart bypass),
- knee replacement
- hysterectomy.
How can this information guide policy and practice?
Understanding where variation is occurring highlights possible areas where the variation may be unwarranted, meaning that it is driven by factors other than patient need or preference.
Unwarranted variation raises questions about efficiency, equity and value in health care.
Without information on clinical and population health outcomes, it is difficult to say if people in some regions are getting more appropriate care than others. Less care is not necessarily worse than more care, and vice versa.
Further investigation is needed into the causes of variation to better understand if patients in particular regions are getting the right level of care, and to pave the way to addressing any problems that are identified. Clinicians, patients and policy makers must be engaged in understanding, interpreting and acting on the data.
How can care be made more appropriate for patient needs and preferences?
There are complementary mechanisms to improve appropriateness in health care, such as shared decision making and improving patients’ health literacy.
Shared decision making is a process that enables patients to better understand their options, and provides an avenue for clinicians to better understand their patients’ needs and preferences. Importantly, shared decision making is a way of incorporating clinical evidence into the consultation.
There is growing evidence suggesting that patients who are better informed about their health care options are more inclined to choose treatment options that are reflective of their preferences, wishes and tolerance of risk.
Sometimes this may result in more conservative treatment choices, and it has been observed that for some conditions, more informed patients tend to be less likely to opt for surgery.
Ultimately, the goal is that the patient and their healthcare provider, together, elicit the patient’s preferences and choose the most appropriate, evidence-based treatment option. This can help reduce unwarranted variation and ensure appropriate care.
The Commission wishes to acknowledge the contribution of Ms Coral Warren, and Ms Lucia Tapsall.