A team of surgeons at New York-Presbyterian/Morgan Stanley Children’s Hospital saved the life of a one-week-old baby with the aid of a 3-D printed model of the child’s heart. The 3-D model was used as a guide for surgery on the child, who was born with a complex and deadly form of congenital heart disease (CHD).
Dr. Emile Bacha, director of congenital and pediatric cardiac surgery at New York-Presbyterian/Morgan Stanley Children’s Hospital (NY-P/MSCH), and his team performed surgery when the baby was just one week old and weighed only 7 lbs. With the aid of the 3-D model, the team was able to repair all of the heart’s defects in a single procedure. Typically, babies born with this complex form of CHD require a series of three or four life-threatening surgeries.
“The baby’s heart had holes, which are not uncommon with CHD, but the heart chambers were also in an unusual formation, rather like a maze,” said Dr. Bacha, who is also chief of the division of cardiac, thoracic and vascular surgery at New York-Presbyterian/Columbia University Medical Center and the Calvin F. Barber Professor of Surgery at Columbia University College of Physicians and Surgeons (P&S).
“In the past, we had to stop the heart and look inside to decide what to do,” he explained. “With 3-D printing technology, we are able to look at the inside of the heart in advance, giving us a road map for the surgery.”
Prior to the surgery, a team of doctors led by Dr. Anjali Chelliah, a pediatric cardiologist at NY-P/MSCH and assistant professor at P&S, diagnosed the baby with CHD while he was still in the womb, allowing time to develop the optimal treatment plan. After the baby was born, Dr. Chelliah worked closely with Materialise–a company that specializes in 3-D printing for healthcare–to create a model of the child’s heart with data taken from a low-dose CT scan performed just one day after the baby’s birth.

Using a special 3-D printer, scientists created a replica of the newborns’ heart based on a series of CT scans taken just one day after the infant was born.
Only two days after receiving the data, the printer was able to produce an exact replica of the heart, allowing the doctors to closely examine and understand every detail of the congenital defects. “After the success of this surgery, it’s clear that 3-D models can be successfully used to help surgeons in complex procedures,” said Dr. Bacha. “This technology is the future, and we are proud that NY-P/MSCH is leading the way.”
The cost of printing the 3-D model of the baby’s heart was paid for by Matthew’s Hearts of Hope, a non-profit organization that supports CHD patients and their families. They have said that another 3D printed heart is in the making, with details to follow in the next month.
Meanwhile, in a very similar procedure just the other day, Kentucky surgeon Dr. Erle Austin also credited 3D printing with improving the odds of succeeding in the most difficult surgeries, reports Wired. “I’m using 3D printing to help me understand a complicated heart,” he told Maker Faire in Rome. Like the team at NY-P/MSCH, Dr. Austin used the technology to inform his approach to heart surgery on a young child at Kosair Children’s Hospital. “If I went in and did surgery, took off the front of the heart and did irreparable damage, the child would not survive,” he said.

Creating a replica of the child’s heart allowed surgeons to explore the organ before performing surgery, which gave them a critical opportunity to plan their surgical approach and greatly reduced the risk of surgical complications.
Using an experimental version of the Makerbot Replicator 2, Dr. Austin printed a copy of the heart in three parts. “Because I have an identical reconstruction I can take off the front of the heart and see inside of it and make a plan as to how I’m going to direct the flow of blood and move the obstruction in the heart.”
What Is 3-D Printing?
Imagine an ink jet printer that, rather than spraying out ink in the shape of letters, sprays out a plastic or metal gel or powder in the shape of a tooth, finger, heart, or any number of other body parts. A typical printer receives a document to print, while 3-D printers take their commands from an MRI or a CT scan of a body part. Also known as “additive manufacturing,” 3-D printing produces an object, layer by layer, from the ground up.

3-D printers use materials such as glass, metal, and plastic, which are then meticulously added layer-by-layer to create a range of implants, fillers, prosthetics, and models like the one used by the surgeons at NY-P/MSCH.
Although 3-D printers have been around since the 1980s, medical uses have only begun to skyrocket in the past few years. The printers can produce more complex shapes than traditional manufacturing, allowing the products to be highly personalized.
The process can save time and practically bring production of medical devices to the patient’s bedside. It can also be substantially less expensive than alternative methods. Although no one has exact numbers, it is estimated that several dozen medical centers in the country now use 3-D printers in some form.
How 3-D Printing Is Advancing Medicine
3-D printing is already widely used to create body parts — usually made of plastic or metal — that come in contact with the body but don’t enter the bloodstream. These include teeth, hearing aid shells, and prosthetic limbs.

These are just a few of the many different body parts that have been successfully designed and created using 3-D printing technology.
However, the technology is now starting to be used to create more complex structures — particularly human tissue. Using special 3-D printers, called bioprinters, scientists can actually print functional human tissue for medical research and regenerative therapies. Instead of the plastic, metal, or glass used in a regular 3-D printer, bioprinters use a “bio-ink” made of living cell mixtures to form human tissue. Basically, the bio-ink is used to build a 3D structure of cells, layer by layer, to form tissue.
Eventually, medical researchers hope to be able to use the printed tissue to make organs for organ replacement, though it will likely be another decade before we see anything like that go into use. But even though developing functional organs may still be years away, medical researchers and others are using bioprinting technology to make advancements in other ways.
Applications of 3-D Printing
Researchers in regenerative medicine at Wake Forest University in North Carolina partnered with the Armed Forces Institute for Regenerative Medicine to make a 3-D skin printer that deposits cells directly on a wound to help it heal quicker. Researchers at the university have also had success printing off kidney cells.

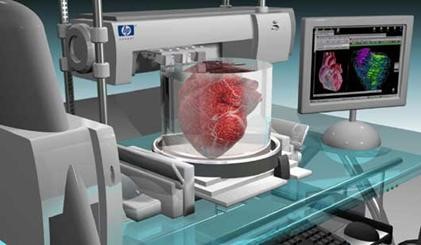
Above, a 3-D printer is shown in the process of printing a human kidney. Although a great deal of research still remains to be done, scientists hope to use the 3-D printers to create organs suitable for transplantation.
Bioengineers at Cornell University have printed experimental knee cartilage, heart valves and bone implants. And the non-medical start-up Modern Meadow, which is backed by investor Peter Thiel, is using bioprinting technology to develop a way to print meat.
Bio-printing is also playing a part in how some pharmaceutical companies conduct medical research, and the technology may also have the potential to save the drug companies a lot of money because it could cut drug testing costs, Chen said.
Medical researchers in the pharmaceutical industry, until lately, have used two-dimensional cell cultures to test drugs during the early stages of development. However, the 2D cell cultures do not reflect human tissue as accurately as 3D printed tissue, meaning the 2D models can create misleading test results. Testing with 3D tissues, however, provide more precise results, which allows for pharmaceutical companies to determine failed drugs early on before investing more money in development.
And with clinical trials accounting for the largest percentage of the biopharmaceutical industry’s budget for the research and development at $31.3 billion, according to a report from the Presidents Council on Science and Technology, it’s no surprise that drug companies want to use 3D tissues to help avoid wasted costs.