Researchers from the UNC School of Medicine have discovered that cells called fibroblasts, which normally give rise to scar tissue after a heart attack, can be turned into endothelial cells, which generate blood vessels to supply oxygen and nutrients to the injured regions of the heart, thus greatly reducing the damage done following heart attack.
This switch is driven by p53, the well-documented tumor-suppressing protein. The UNC researchers showed that increasing the level of p53 in scar-forming cells significantly reduced scarring and improved heart function after heart attack.
The finding, which was published today in the journal Nature, shows that it is possible to limit the damage wrought by heart attacks, which strike nearly one million people in the United States each year. Heart disease accounts for one in four deaths every year.
“Scientists have thought that fibroblasts are terminally differentiated, meaning they can’t adopt the fate of other kinds of cells; but our study suggests this may not be entirely true,” said Eric Ubil, PhD, a postdoctoral fellow at UNC and first author of the Nature study. “It appears that injury itself can induce fibroblasts to change into endothelial cells so the heart heals better. We found a drug that could push this process forward, making even more endothelial cells that help form blood vessels. The results were truly amazing in mice, and it will be exciting to see if people respond in the same way.”
After a heart attack, fibroblasts replace damaged heart muscle with scar tissue. This scarring can harden the walls of the heart and lessen its ability to pump blood throughout the body. Meanwhile, endothelial cells create new blood vessels to improve circulation to the damaged area. However, sometimes these endothelial cells naturally turn into fibroblasts instead, adding to the scarring.
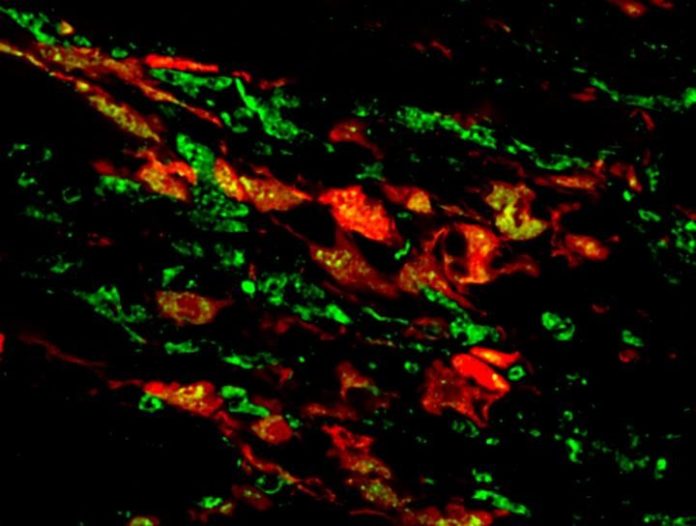
Ubil and his colleagues wondered if the switch ever flipped the other way — could fibroblasts turn into endothelial cells. To explore this idea, they induced heart attacks in mice and then studied the fibroblasts to see if the cells expressed markers characteristic of endothelial cells. To their surprise, almost a third of the fibroblasts in the area of the cardiac injury expressed these endothelial markers. The researchers found that the endothelial cells generated from fibroblasts actually gave rise to functioning blood vessels.
Next, Ubil and colleagues wanted to identify the molecule that triggered the switch. Because a heart attack is such a stressful event, Ubil created a list of genes that were known to be involved in cellular responses to stress. Topping the list was p53, a protein often called the “guardian of the genome” because it causes damaged, out of control cells to commit suicide, or apoptosis, which reduces the likelihood that they will go on to form tumors.
“As luck would have it, that was the first gene I tried, and that was the last gene I tried,” said Ubil, who conducted the research as a graduate student in the laboratory of former UNC faculty member and senior study author Arjun Deb, MD.
Ubil found that p53 was “turned on” or overexpressed in the fibroblasts after heart injury and this seemed to regulate fibroblasts becoming endothelial cells. He and colleagues figured that if the p53 protein was responsible for the positive switch, then blocking it in mice would halt the transition from scar-forming cells to blood vessel-forming cells. Their experiments revealed that knocking out the p53 gene in scar-forming cells in adult mice decreased the number of cells making the switch by 50 percent.
Likewise, the researchers rationalized that upping the level of p53 would increase the number of fibroblasts that would turn into endothelial cells. Because p53 is often mutated or lost in cancer cells, a number of compounds have been designed to increase its levels as a possible anti-cancer treatment. The researchers picked one such experimental drug called RITA — Reactivation of p53 and Induction of Tumor cell Apoptosis — and used it to treat mice for a few days after cardiac injury. The drug had dramatic results, doubling the number of fibroblasts that turned into endothelial cells. That is, instead of just 30 percent of fibroblasts naturally switching into endothelial cells, 60 percent made the switch.
“The treated mice benefited tremendously,” Ubil said. “There was such a huge decrease in scar formation. We checked the mice periodically, from three days to fourteen days after treatment. They had more blood vessels at the site of injury, and their heart function was better. By increasing the number of blood vessels in the injury region, we were able to greatly reduce the effects of the heart attack.”
Ubil said his study shows that this could be a novel strategy for treating heart attacks. However, he cautioned that any treatments based on the discovery outlined in Nature are many years away.
“But our work shows it’s possible to change the fate of scar-forming cells in the heart, and this could potentially benefit people who have heart attacks,” Ubil said.
Deb added, “We are also currently investigating whether such an approach could be applied for treating scarring in other organs after injury.”
The research was supported by the American Heart Association and the National Institutes of Health.
Eric Ubil, PhD, is now a postdoctoral fellow at the UNC Lineberger Comprehensive Cancer center. Other UNC co-authors include graduate student Francesca Bargiacchi and Mauricio Rojas, MD, MPH. Arjun Deb, MD, is now on the faculty at UCLA.
Story Source:
The above story is based on materials provided by University of North Carolina School of Medicine. Note: Materials may be edited for content and length.
Journal Reference:
- Eric Ubil, Jinzhu Duan, Indulekha C. L. Pillai, Manuel Rosa-Garrido, Yong Wu, Francesca Bargiacchi, Yan Lu, Seta Stanbouly, Jie Huang, Mauricio Rojas, Thomas M. Vondriska, Enrico Stefani, Arjun Deb. Mesenchymal–endothelial transition contributes to cardiac neovascularization. Nature, 2014; DOI: 10.1038/nature13839