Fatigue, weight gain, chills, hair loss, anxiety, excessive perspiration — these symptoms are a few of the signs that the thyroid gland, which regulates the body’s heart rate and plays a crucial role in its metabolism, has gone haywire. Now, new research from Tel Aviv University points to an additional complication caused by thyroid imbalance: congenital deafness.
The study, published in Mammalian Genome, was conducted by Prof. Karen B. Avraham and Dr. Amiel Dror of the Department of Human Molecular Genetics and Biochemistry at TAU’s Sackler School of Medicine. Using state-of-the-art imaging, the researchers found that congenital deafness can be caused by an absence of a thyroid hormone during development.
“Since our laboratory mainly focuses on the system of the inner ear, the study of a system such as the thyroid gland was new to us and therefore challenging,” said Dr. Dror. “My curiosity as to how these two systems interact together to develop normal hearing led to this multidisciplinary study.”
A colorful approach
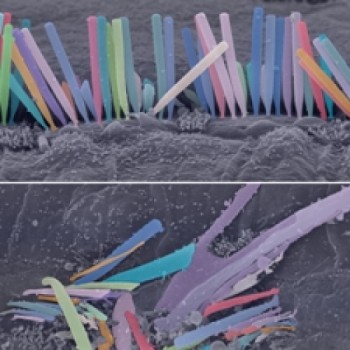
The researchers used mouse populations to study a form of congenital deafness that affects humans. Harnessing electron microscopy at the Sackler Cellular & Molecular Imaging Center, researchers tracked the inner hair cells of the cochlea (the auditory portion of the inner ear) in two groups — control (wild) mice and mutant (congenitally deaf) mice. Inner-ear hair bundles in the affected mice were labelled with bright colors to highlight the disorganization of the ear’s hair cells.
Examination of the inner ear showed a spectrum of structural and molecular defects consistent with hypothyroidism or disrupted thyroid hormone action. The researchers’ analysis of the images revealed defective formation of the mice’s thyroid glands: labelled thyroid follicles did not grow or grew incompletely.
“Our work demonstrated that normal hearing fails to develop when thyroid hormone availability is insufficient as a result of a genetic mutation,” said Dr. Dror. “Our model provides a platform to test therapeutic approaches in order to prevent hearing loss before it occurs. There is still long way ahead before we get to the point of practical treatments with our research, but we believe we are moving in the right direction.”
A lifelong commitment
“My attraction to sound began very early as a child,” said Dr. Dror. “I play string instruments and pay great attention to sound quality and perception. As a graduate student in the Avraham laboratory, I was exposed to the fascinating world of genetics and the opportunity to combine two fields of research that I am interested in: genetics and hearing. Now that I have continued this research as a medical student, the direct interaction with patients with hearing impairments encouraged me to explore the clinical significance of my research.”
As a physician, Dr. Dror believes it is important to pursue research with clinical consequences for his patients. “The basis of all advanced medicine relies on both basic science and clinical research. I hope that our study will contribute a modest part to global efforts for improved medical care and treatment of hearing impairments,” Dr. Dror said.
Story Source:
The above story is based on materials provided by American Friends of Tel Aviv University. Note: Materials may be edited for content and length.
Journal Reference:
- Amiel A. Dror, Danielle R. Lenz, Shaked Shivatzki, Keren Cohen, Osnat Ashur-Fabian, Karen B. Avraham. Atrophic thyroid follicles and inner ear defects reminiscent of cochlear hypothyroidism in Slc26a4-related deafness. Mammalian Genome, 2014; 25 (7-8): 304 DOI: 10.1007/s00335-014-9515-1