Transmission of bacterial infections, including MRSA and MSSA could be curbed by coating hospital surfaces with microscopic bumps that mimic the scaly surface of shark skin, according to research published in the open access journal Antimicrobial Resistance and Infection Control.
The study modelled how well different materials prevented the spread of human disease bacteria through touching, sneezes or spillages. The micropattern, named Sharklet™, is an arrangement of ridges formulated to resemble shark skin. The study showed that Sharklet harboured 94% less MRSA bacteria than a smooth surface, and fared better than copper, a leading antimicrobial material. The bacteria were less able to attach to Sharklet’s imperceptibly textured surface, suggesting it could reduce the spread of superbugs in hospital settings.
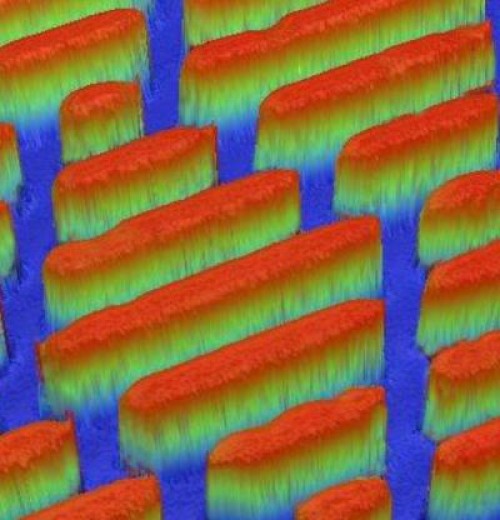
The surfaces in hospitals and healthcare settings are often rife with bacteria and patients are vulnerable to bacterial infection. Scientists are investigating the ability of different materials to prevent the spread of bacteria. Copper alloys are a popular option, as they are toxic to bacterial cells, interfering with their cellular processes and killing them. The Sharklet micropattern works differently — the size and composition of its microscopic features prevent bacteria from attaching to it. It mimics the unique qualities of shark skin, which, unlike other underwater surfaces, inhibits bacteria, because it is covered with a natural micropattern of tooth-like structures, called denticles.
Dr Ethan Mann, a research scientist at Sharklet Technologies, the manufacturer of the micropattern, says: “The Sharklet texture is designed to be manufactured directly into the surfaces of plastic products that surround patients in hospital, including environmental surfaces as well as medical devices. Sharklet does not introduce new materials or coatings — it simply alters the shape and texture of existing materials to create surface properties that are unfavorable for bacterial contamination.”
The researchers from Sharklet Technologies compared how well two types of infection-causing bacteria, methicillin-resistant or susceptible Staphylococcus aureus (MRSA and MSSA), fared at contaminating three surfaces — the Sharklet micropattern, a copper alloy, and a smooth control surface. They created experimental procedures to mimic common ways bacteria infect surfaces. Sneezing was mimicked by using a paint sprayer to spread the bacterial solution on 10 samples of each surface. To mimic infected patients touching the surfaces, velveteen cloth was put in contact with bacteria for 10s, and then placed on another set of each test surface for 10s. A third set of each surface was immersed in bacterial solution for an hour, then rinsed and dried, to mimic spills.
Surfaces were sampled for remaining contaminations either immediately following exposure to MSSA and MRSA or 90 minutes after being exposed. The Sharklet micropattern reduced transmission of MSSA by 97% compared to the smooth control, while copper was no better than the control. The micropattern also harboured 94% less MRSA bacteria than the control surface, while the copper had 80% less.
Dr Mann says: “Shark skin itself is not an antimicrobial surface, rather it seems highly adapted to resist attachment of living organisms such as algae and barnacles. Shark skin has a specific roughness and certain properties that deter marine organisms from attaching to the skin surface. We have learned much from nature in building this material texture for the future.”
Story Source:
The above story is based on materials provided by BioMed Central. Note: Materials may be edited for content and length.
Journal Reference:
- Ethan E Mann, Dipankar Manna, Michael R Mettetal, Rhea M May, Elisa M Dannemiller, Kenneth K Chung, Anthony B Brennan, Shravanthi T Reddy. Surface micropattern limits bacterial contamination. Antimicrobial Resistance and Infection Control, 2014; 3 (1): 28 DOI: 10.1186/2047-2994-3-28