A peek inside the brains of more than 750 children and teens reveals a key difference in brain architecture between those with attention deficit hyperactivity disorder and those without.
Kids and teens with ADHD, a new study finds, lag behind others of the same age in how quickly their brains form connections within, and between, key brain networks.
The result: less-mature connections between a brain network that controls internally-directed thought (such as daydreaming) and networks that allow a person to focus on externally-directed tasks. That lag in connection development may help explain why people with ADHD get easily distracted or struggle to stay focused.
What’s more, the new findings, and the methods used to make them, may one day allow doctors to use brain scans to diagnose ADHD — and track how well someone responds to treatment. This kind of neuroimaging “biomarker” doesn’t yet exist for ADHD, or any psychiatric condition for that matter.
The new findings come from a team in the University of Michigan Medical School’s Department of Psychiatry. They used highly advanced computing techniques to analyze a large pool of detailed brain scans that were publicly shared for scientists to study. Their results are published in the Proceedings of the National Academy of Sciences.
Lead author Chandra Sripada, M.D., Ph.D., and colleagues looked at the brain scans of 275 kids and teens with ADHD, and 481others without it, using “connectomic” methods that can map interconnectivity between networks in the brain.
The scans, made using function magnetic resonance imaging (fMRI) scanners, show brain activity during a resting state. This allows researchers to see how a number of different brain networks, each specialized for certain types of functions, were “talking” within and amongst themselves.
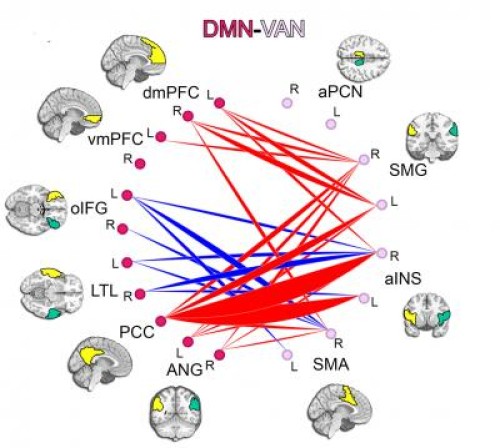
The researchers found lags in development of connection within the internally-focused network, called the default mode network or DMN, and in development of connections between DMN and two networks that process externally-focused tasks, often called task-positive networks, or TPNs. They could even see that the lags in connection development with the two task-related networks — the frontoparietal and ventral attention networks — were located primarily in two specific areas of the brain.
The new findings mesh well with what other researchers have found by examining the physical structure of the brains of people with and without ADHD in other ways.
Such research has already shown alterations in regions within DMN and TPNs. So, the new findings build on that understanding and add to it.
The findings are also relevant to thinking about the longitudinal course of ADHD from childhood to adulthood. For instance, some children and teens “grow out” of the disorder, while for others the disorder persists throughout adulthood. Future studies of brain network maturation in ADHD could shed light into the neural basis for this difference.
“We and others are interested in understanding the neural mechanisms of ADHD in hopes that we can contribute to better diagnosis and treatment,” says Sripada, an assistant professor and psychiatrist who holds a joint appointment in the U-M Philosophy department and is a member of the U-M Center for Computational Medicine and Bioinformatics. “But without the database of fMRI images, and the spirit of collaboration that allowed them to be compiled and shared, we would never have reached this point.”
Sripada explains that in the last decade, functional medical imaging has revealed that the human brain is functionally organized into large-scale connectivity networks. These networks, and the connections between them, mature throughout early childhood all the way to young adulthood. “It is particularly noteworthy that the networks we found to have lagging maturation in ADHD are linked to the very behaviors that are the symptoms of ADHD,” he says.
Studying the vast array of connections in the brain, a field called connectomics, requires scientists to be able to parse through not just the one-to-one communications between two specific brain regions, but the patterns of communication among thousands of nodes within the brain. This requires major computing power and access to massive amounts of data — which makes the open sharing of fMRI images so important.
“The results of this study set the stage for the next phase of this research, which is to examine individual components of the networks that have the maturational lag,” he says. “This study provides a coarse-grained understanding, and now we want to examine this phenomenon in a more fine-grained way that might lead us to a true biological marker, or neuromarker, for ADHD.”
Sripada also notes that connectomics could be used to examine other disorders with roots in brain connectivity — including autism, which some evidence has suggested stems from over-maturation of some brain networks, and schizophrenia, which may arise from abnormal connections. Pooling more fMRI data from people with these conditions, and depression, anxiety, bipolar disorder and more could boost connectomics studies in those fields.
Volunteers needed for research:
To develop such a neuromarker, Sripada has embarked on follow-up research. One study is enrolling children between the ages of 7 and 17 who have ADHD and a comparison group of those without it; information is at http://umhealth.me/adhdchild. Another study is enrolling adults between the ages of 18 and 35 who have ADHD and a comparison group of those without it; information is at http://umhealth.me/adhdadult. Of note, fMRI scans do not expose a person to radiation. Anyone interested in these studies can email Psych-study@med.umich.edu or call (734) 232-0353; for the study of children, parents should make the contact and consent to research on behalf of their children.=
Story Source:
The above story is based on materials provided by University of Michigan Health System. Note: Materials may be edited for content and length.
Journal Reference:
- Chandra S. Sripada, Daniel Kessler, And Mike Angstadt. Lag in maturation of the brain’s intrinsic functional architecture in attention-deficit/hyperactivity disorder. PNAS, September 2014 DOI: 10.1073/pnas.1407787111